Depression or Anxiety — or Both? Understanding the Overlap

We often think of anxiety and depression as opposites. After all, one causes excessive worrying and jitters while the other leads to a lack of energy and motivation. But despite the differences between anxiety and depression, the two overlap quite often, making it hard to determine if you’re experiencing anxiety, depression, or both. This guide can help decipher what’s causing your symptoms, help you recognize the signs of anxiety and depression, and offer effective treatment options.
“I have what?” I said to my therapist, not sure I had heard her right. She repeated that I had both anxiety and depression, which didn’t quite compute in my brain. After all, there’s a big difference between anxiety and depression. One causes uncontrollable worrying and nervous energy. The other leads to a hopeless mood and lack of motivation.
At the time of diagnosis, it’s hard to wrap your brain around two diagnoses, much less imagine that one treatment plan can address both. Luckily, I worked with a brilliant mental healthcare provider who helped me understand the differences between anxiety and depression, as well as how to get both into remission.
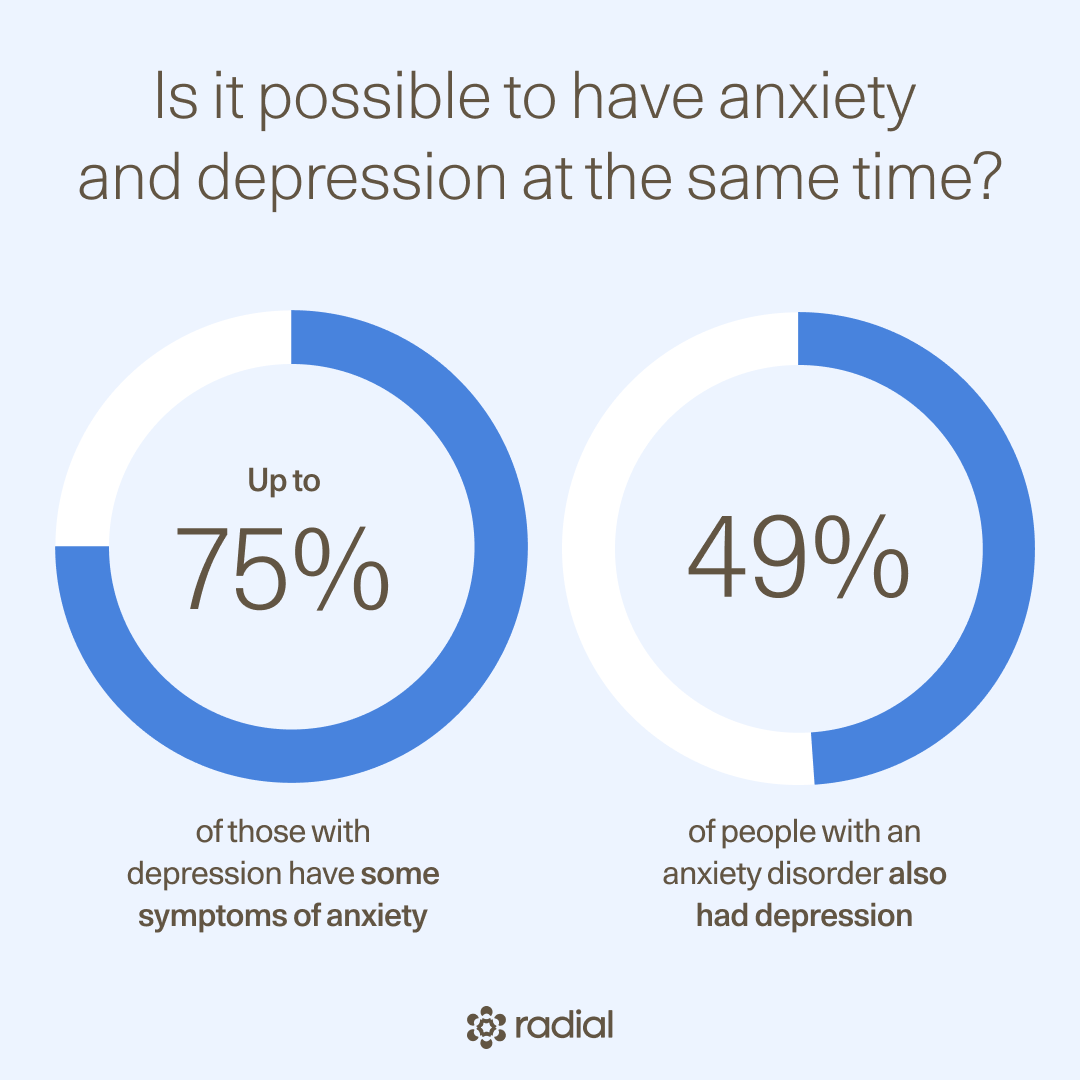
And my story isn’t all that unique—having anxiety and depression is quite common, with some studies finding up to 75% of patients with major depressive disorder also experience symptoms of anxiety. There are also many success stories for treating depression and anxiety, and it’s possible to build a life of joy and purpose after being diagnosed with one or both.
In this guide, we’ll overview the core differences between depression and anxiety, where these conditions overlap, and what the road to diagnosis and recovery looks like. Most importantly, you’ll be able to identify what next step is right for you, whether that looks like reaching out to a mental healthcare provider or exploring a new-to-you treatment.
What is anxiety?
Our brains are actually designed to feel anxious or nervous when we face a threat. Feelings of anxiety can trigger our fight-or-flight response, which is what allowed our ancestors to escape predators or fight off danger. In our modern world, we’re (hopefully) not being chased by lions, but our brains still provide similar responses when we face any stressor, which could range in severity from a life-threatening event to a frustrating work email.
When that stress response is triggered often by things that aren’t life-threatening or the response is hard to shut off, it is often a sign of an anxiety disorder. “Anxiety is basically the fear or threat detection center running wild,” says Maryellen Eller, MD, a board-certified adult psychiatrist.
That center is more formally referred to as the amygdala, which is the part of the brain that sounds the alarm when we detect a threat. The amygdala then communicates that fear to the prefrontal cortex, the decision maker in the brain, who decides if the threat is worth acting on.
“In anxiety disorders, the amygdala starts sending extra threat signals, and our prefrontal cortex gets weaker or has a harder time evaluating what we should do with that threat,” explains Dr. Eller, “So we end up with this runaway threat response system.”
That runaway response system affects our minds and bodies in many ways:
- Feeling restless, easily frustrated, or irritable
- Intrusive, anxious thoughts
- Intense fear
- Excessive worrying
- Feeling on edge
- Pounding or rapid heartbeat
- Physical tension
- Unexplained aches
- Shortness of breath
- Difficulty concentrating
- Dizziness
- Upset or anxious stomach
- Trouble falling or staying asleep
About one-third of Americans will experience an anxiety disorder at least once in their life. While most share the symptoms above, there are multiple types of anxiety disorders, each with distinct characteristics:
- Generalized anxiety disorder: When someone feels severe, frequent worry for months or even years without a specific cause.
- Panic disorders: When someone experiences unexpected panic attacks, which are sudden feelings of terror when no danger is present.
- Phobia-related anxieties: When someone has an anxiety related to a specific fear, such as tight spaces or needles.
- Social anxiety disorder: When someone experiences a strong sense of dread in social situations.
- Postpartum anxiety: Intense worry after having a baby that is hard to shut off.
What is depression?
Have you ever had a to-do list so long you feel like shutting down? That sensation is similar to depression, except depression leads to a much more severe reaction than everyday overwhelm.
Like with anxiety, the amygdala goes into overdrive when someone is depressed. Unlike with anxiety, depression also directly impacts the prefrontal cortex, which means our decision-making functions aren’t working as well when depressed, and the hippocampus, the part of the brain responsible for storing memories, which is why many with depression experience a brain fog. Dr. Eller adds, “The parts of our brain that get stuck in thought patterns like rumination, self criticism, and hopelessness also become overactive.”
When someone is depressed, the brain also releases less dopamine, the reward chemical. Depression also leads to the dysregulation of serotonin, a neurotransmitter that helps us regulate mood, and a decrease in norepinephrine, a neurotransmitter that helps us with cognitive function and responding to stressors.
Together, these alterations to how the brain and neurotransmitters operate take the form of an intense feeling of sadness—and intense is the keyword here. It’s not just a day when you feel a bit sad, but a debilitating melancholy.
True depression manifests in someone’s mood, thoughts, and body:
- Feeling irritable, restless, or easily frustrated
- Disinterest in old hobbies and passions
- Feeling sad or anxious often
- Trouble falling or staying asleep
- Sleeping too much once asleep
- Eating too much or having no appetite
- Unexplained aches
- Unexplained stomach problems
- Feeling fatigued, even after a good night’s rest
- Feeling unmotivated
- Difficulty concentrating
- Feeling hopeless, guilty, or worthless
Like with anxiety, there are also different types of depression:
- Major depressive disorder (MDD): A disorder where feelings of hopelessness and sadness interfere with everyday life.
- Persistent depressive disorder: When someone has less severe symptoms of depression, but they last for at least two years.
- Seasonal affective disorder (SAD): When symptoms come and go with the changing of the seasons. SAD typically starts in fall, lasts through winter, and ends in spring.
- Bipolar depression: Part of bipolar disorder, a mood disorder where someone has episodes of depression that feature many of the same symptoms as MDD, and episodes of mania or hypomania, (with healthy episodes between).
- Postpartum depression: Intense sadness after having a baby that’s caused, in part, by a dramatic drop in certain hormones during childbirth.
- Depression with psychosis: When depressive symptoms are accompanied by false beliefs and/or seeing, feeling, or hearing something that isn’t there.
What’s the difference between anxiety and depression?
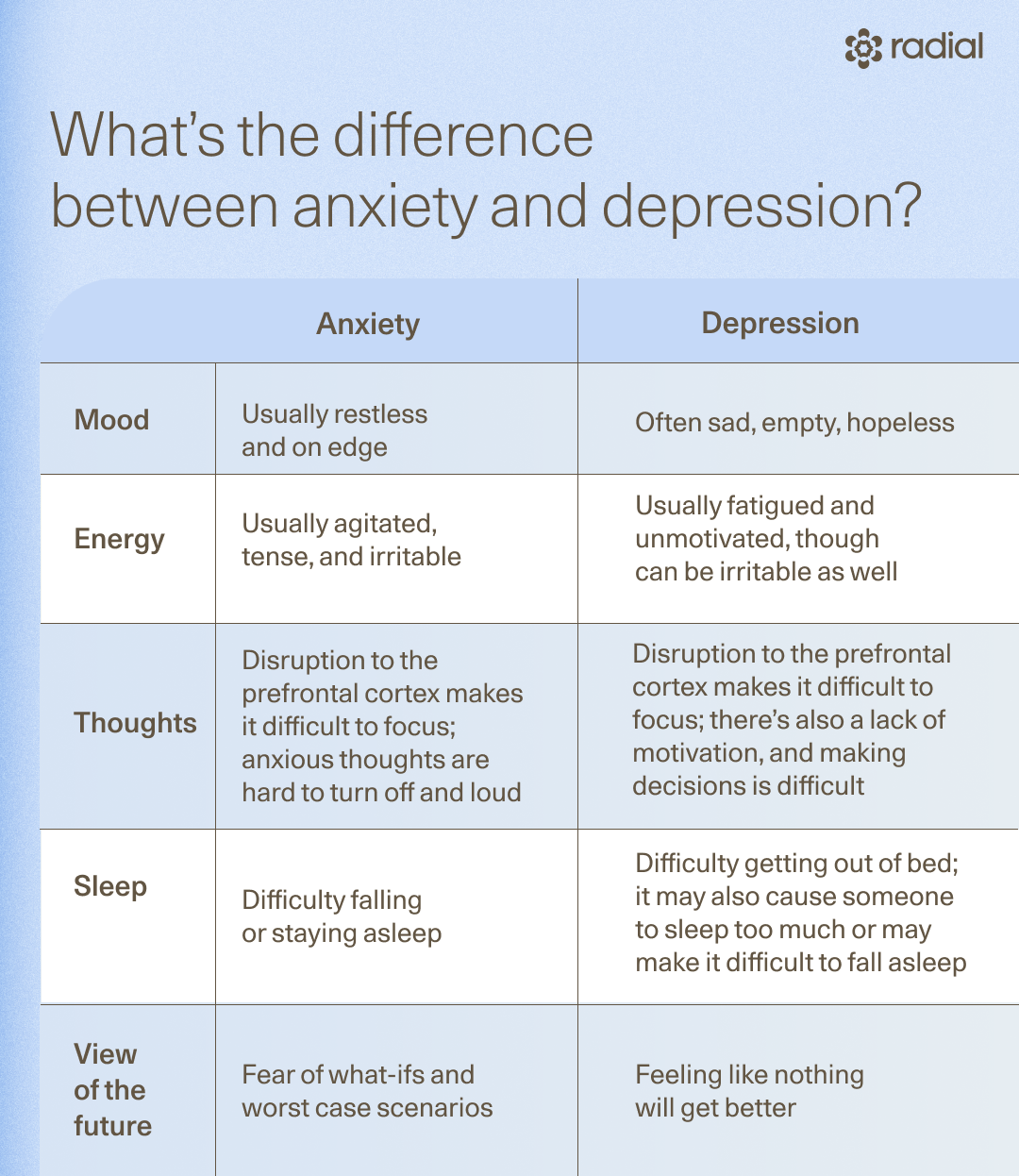
Some of the key characteristics of anxiety vs depression are quite easy to identify, at least in theory. “Oftentimes with anxiety, what people will describe is the sense of restlessness, increased energy in their body that they don't know what to do with,” says Dr. Eller. In contrast, she often thinks of depression as hibernation mode. It often feels like the brain is running on 10% battery—there’s low energy, minimal motivation, and people feel stuck.
The two conditions impact how we think differently too. With anxiety, the brain won’t shut off. It’s constantly spiraling into what-ifs, mistakes you made, and all the bad things that might happen. Depression can also lead to negative spirals, though they’re marked by “cycles of feeling hopeless, catastrophic thinking, and really negative self-talk. It’s very much an internalized negative voice that won't quit,” says Dr. Eller.
How do clinicians tell the difference?
When clinicians are determining if someone has anxiety or depression (or both), they’ll probably ask about the symptoms someone is experiencing, including how long they have lasted and how they impact everyday life.
This information not only helps a mental health provider decide on if it’s depression vs anxiety or if someone has both, it provides clues about the severity, what type of depression or anxiety it is, and what treatment for depression and anxiety may work best. Mental healthcare providers may also use a screening tool to confirm any diagnoses.
Depression
- Beck Depression Inventory (BDI)
- Hamilton Rating Scale for Depression (HAM-D)
- Patient Health Questionnaire-9 (PHQ-9)
Anxiety
Where do anxiety and depression overlap—and is it possible to have both?
While these conditions manifest differently, they are both exacerbated by chronic stress. “It is incredibly common for people to have both [anxiety and depression],” Dr. Eller explains, “And a big takeaway is, if you're depressed and/or anxious, or you have both, you're not broken. Your brain is doing exactly what your brain should do to try and protect you from chronic stress.”
It’s important to note that chronic stress alone doesn’t cause anxiety and depression, and not everyone who experiences stress will develop one or both of these conditions. Both seem to stem from a combination of stress, genetics, environmental factors, and brain chemistry imbalances.
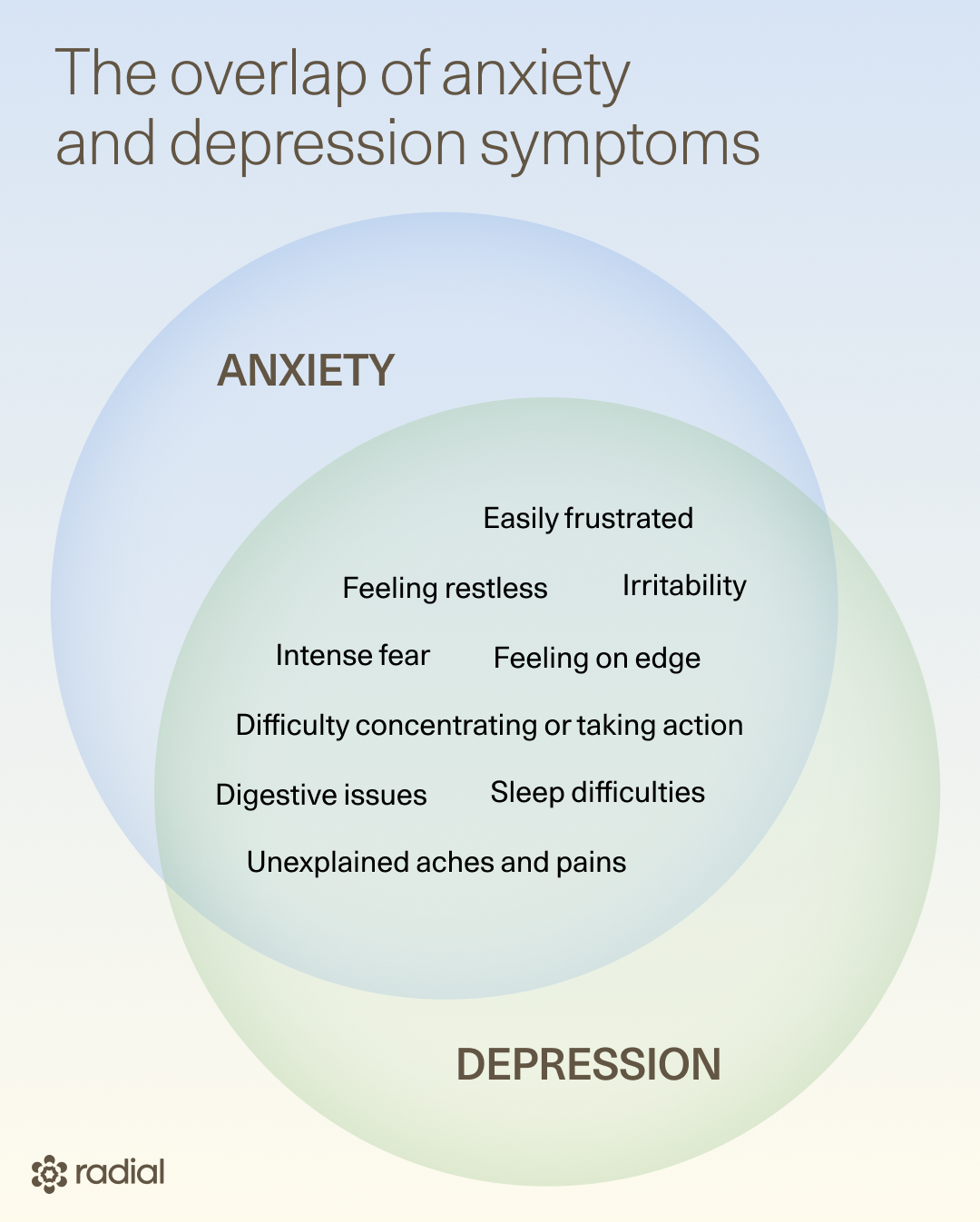
They share other similarities too, such as the involvement of the amygdala and prefrontal cortex and some similar treatment options, which we’ll outline in the next section.
There’s also a fair amount of cross-over in the emotional and physical symptoms of anxiety and depression. Those they share include:
- Being easily frustrated
- Feeling restless
- Irritability
- Feeling on edge
- Intense fear
- Difficulty concentrating or taking action
- Digestive issues
- Sleep difficulties
- Unexplained aches and pains
Is it possible to have anxiety and depression at the same time?
Having both anxiety and depression is not only possible, but common: up to 75% of those with MDD have some symptoms of anxiety (though not a diagnosed anxiety disorder), and in one study, 49% of people with an anxiety disorder also had depression.
When someone has both as part of the same syndrome, it’s referred to as anxious depression, mixed anxiety-depressive (MADD) disorder, or major depressive disorder with anxious distress. People in this state often feel tired but wired. Their brain has an abundance of nervous energy yet is unmotivated and dread-filled. In other cases, two distinct diagnoses are made, for example, a major depressive disorder and a generalized anxiety disorder. Dr. Eller adds that patients with comorbid anxiety and depression often feel extremely stuck and overwhelmed.
Treatment options for anxiety, depression, and both
“Anxious depression is a little more difficult to treat than just plain anxiety or plain depression,” Dr. Eller says. When treating depression with anxiety, Dr. Eller often pulls treatments from a few boxes: psychotherapy, medications, neuromodulation techniques, and lifestyle changes.
Psychotherapy
While chronic stress is the underlying cause of both depression and anxiety, we can’t entirely cut out stress from our lives. We can, however, learn how to respond to it differently, and that’s where therapy for depression and anxiety comes in.
Imagine two people are running the same 5K race. One person is so nervous, they stay up all night. By the time they get to the start line, their sleep-deprived brain imagines worst case scenarios, and negative self talk is on repeat.
The other person feels like the race is a challenge but reminds themselves that they are prepared. They may even silently congratulate themselves for just showing up. Odds are, the second person will have a more fun race (and may even run faster).
Both runners experience the same stressor, but they react differently. Therapy is the coaching that can get you to think and respond to stressors like that second runner, even when facing stress and depression.
And there’s a lot of overlap between the best therapeutic approaches for anxiety and depression, meaning your therapist may use one framework to address both:
- Cognitive behavioral therapy (CBT): Helps identify and reframe negative thoughts and behaviors, and can be used for depression, anxiety, or both.
- Acceptance and commitment therapy (ACT): Encourages someone to accept negative thoughts and recommit to their goals. This therapy may help with both conditions.
- Mindfulness-based therapy: A therapeutic approach that combines CBT with mindfulness. Some studies suggest this type is more effective than CBT for anxious depression.
- Interpersonal Therapy (IPT): Focuses on improving relationships. IPT is especially useful when depression or anxiety stems from social situations or relationships with others.
Neuromodulation
With both anxiety and depression, circuits in the brain are working differently than intended. Neuromodulation therapies act as a GPS, guiding those neurons so they can better support mood regulation, our thought processes, and other parts of the brain that anxiety and depression disrupt. Two tried-and-true neuromodulation techniques that may work for both are TMS and PRISM.
During transcranial magnetic stimulation (TMS), an electromagnetic device in the shape of a cap or paddle is placed near the head. This device houses a coil that induces tiny electrical currents that target specific regions of the brain, fine-tuning mood-related neurons.
Admittedly, that sounds a bit strange (or at least different from treatments we’re more familiar with) but TMS’ uniqueness is part of why it delivers a much higher remission rate than traditional antidepressants, especially for treatment-resistant depression. It’s also noninvasive, FDA-cleared, and has minimal side effects.
There is, however, one catch: while there’s a lot more evidence to support TMS for depression, its role for anxiety alone is a bit underexplored. That said, experienced TMS providers like Radial have established protocols for TMS therapy for anxious depression.
“There are specific TMS protocols that can target the overlap area for both the anxiety and the depression,” explains Dr. Eller, “By targeting the area in the prefrontal cortex, where those circuits overlap, we can get significant improvement in both the circuit function for anxiety and depression.”
And now to the other part of our neuromodulation alphabet soup: PRISM. You can think of it as a gamified way to overcome depression, anxiety, or both. For this FDA-cleared, noninvasive treatment, you play a video game while wearing an EEG cap that monitors your brain waves. As you go about the game, the cap monitors brain activity and lets you level up when you develop new skills or patterns of thinking.
“Neurofeedback can also be really helpful in the overlap of symptoms,” says Dr. Eller. That’s because it works to calm down the amygdala while also targeting parts of the brain responsible for depression’s numbness and disconnection.
Medication
There are many medications for depression and anxiety:
- Selective serotonin reuptake inhibitors (SSRIs): One of two traditional antidepressant drug classes that helps regulate serotonin.
- Serotonin and norepinephrine reuptake inhibitors (SNRIs): The other traditional antidepressant class that helps regulate norepinephrine as well as serotonin.
- Wellbutrin (bupropion): Targets receptors for dopamine, serotonin, and norepinephrine, reducing the likelihood of depressive thoughts.
- Auvelity (bupropion/dextromethorphan): A combination medication with bupropion (covered in last bullet) and dextromethorphan, which target other neurotransmitters affected by depression.
- Spravato (esketamine): A newer medication with a similar anti-depressant effect. It typically works faster than other medications.
SSRIs and SNRIs, while commonly referred to as “anti-depressants,” are quite effective for anxiety. There is some evidence that they may actually be more effective for anxiety than they are for treating depression. However, psychiatrists also prescribe anti-anxiety medications, like benzodiazepines and buspirone, for anxiety disorders.
Bupropion and Auvelity both list anxiety as a potential side effect, making them a less–than-ideal option for anxious depression or anxiety. While SSRIs, SNRIs, and anti-anxiety medications are good options for some with both conditions, they all work slowly and come with some difficult-to-tolerate side effects.
That leaves us with ketamine and Spravato, or esketamine, which work faster than other medications. “Because of how ketamine works at the glutamate level,” explains Dr. Eller, ”It can target depression symptoms, and it can also help with that stuck thinking pattern that happens in anxiety.”
Lifestyle changes
Most of us probably are aware that healthy habits help with both depression and anxiety, but there’s nothing more frustrating than someone telling you to “stress less” or “be happy” when you’re struggling with your mental health.
While it’s best to ignore advice that belongs on an inspirational pillow, there are evidence-backed lifestyle changes that can help with both:
- Eat an anti-inflammatory diet: You’ve probably eaten a meal that left you feeling extremely sluggish or felt jittery from too much coffee. Turns out, what we eat impacts our mood. A diet that prioritizes feel-good foods (aka anti-inflammatory foods like fruits, veggies, walnuts, fish, and brown rice) has been associated with a decreased risk of anxiety and depression and may help someone manage symptoms of either or both.
- Exercise: Working out is a mood-booster for depression and can calm anxious thoughts. This applies to all types of exercise, meaning you can choose something intense, like a CrossFit class, opt for a more lowkey yoga class, or even go on a quick walk.
- Breathwork: When we’re anxious or depressed, the amygdala becomes hyperactive. Focusing on the breath can help regulate the amygdala and calm feelings of anxiety or depression. And when we say breathwork, we mean more than just breathing. Instead, it’s the practice of breathing in a certain pattern. Wim Hoff’s free 10-minute guided breathing session has personally helped me when feelings of depression or anxiety pop up.
- Light exposure: The Beatles were onto something when they sang, “Here comes the sun.” Daily exposure to sunlight can help improve overall mood and may even reduce anxiety and depression symptoms. If you live somewhere with a cold, dark winter, bright light therapy (aka SAD lamps) may be a solid substitute.
When (and how) to seek help
If symptoms interfere with daily life, seek help. A mental healthcare provider can help you navigate treatment options and decide on the best ones for you. For a wider array of treatment options and faster recovery times, work with an innovative provider who stays up-to-date on newer treatments and the most recent research, such as the team at Radial.
If you’re experiencing suicidal ideation (which is associated with severe anxiety and depression), turn to more immediate crisis resources, such as calling the 988 Suicide & Crisis Lifeline. For the maternal mental health line, call or text 1-833-TLC-MAMA (833-852-6262)
The bottom line
Anxiety and depression can occur separately or together. Both are highly treatable, typically via a combination of psychotherapy, medication, neuromodulation therapies, and lifestyle changes. That said, navigating treatment options can be confusing, which is why it’s important to find the right provider to guide your treatment. The team at Radial regularly supports people in figuring out whether they have anxiety, depression, or both and throughout their recovery journey.
Key takeaways
- Anxiety is commonly defined as excessive worrying or feeling on edge. Depression is prolonged sadness, hopelessness, and low energy. The two can occur separately or together.
- A mental healthcare provider, like the team at Radial, can diagnose someone with one or both and find the right treatment options for your unique situation.
- Both anxiety and depression are treatable. Often, a multi-pronged treatment approach that involves talk therapy, lifestyle changes, medications, and/or neuromodulation therapies works best.
Frequently asked questions (FAQs)
Can anxiety cause depression?
Anxiety can contribute to the development of depression. Living with anxiety leads to fatigue, exhaustion, and sometimes a lack of motivation. Over time, these symptoms may lead to depression.
Can depression cause anxiety?
Depression can cause anxiety, and it’s common for these conditions to co-occur. People with depression often experience worry, restlessness, and anxious thoughts about their situation, and the two conditions impact many of the same areas of the brain.
What causes depression and anxiety?
Both anxiety and depression result from difficulty tolerating chronic stress. However, not everyone who experiences chronic stress will develop anxiety and/or depression. That’s because the cause of both is nuanced and multi-faceted, with genetics, brain chemistry imbalances, and environmental triggers all playing a role.
Deep dive recommendations
- The Frontier Psychiatrists. The Scalable Depression Solution. https://open.substack.com/pub/thefrontierpsychiatrists/p/the-scalable-depression-solution?r=1ct8f&utm_campaign=post&utm_medium=web&showWelcomeOnShare=false
- Psychofarm Podcast. The Deficit Model & Difficult to Treat Depression Featuring Dr. Chris Aiken. https://youtu.be/oj1j2fHq5Gw?feature=shared
- The Frontier Psychiatrists. Generalized Anxiety Disorder: A Dissent. https://thefrontierpsychiatrists.substack.com/p/generalized-anxiety-disorder-a-dissent
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




