Understanding the Differences Between Bipolar 1 and Bipolar 2
You’ve probably heard of bipolar disorder, but what exactly is the difference between bipolar 1 vs 2? The answer is nuanced and important, since the diagnostic criteria and best treatments vary depending on the type of bipolar disorder.
The most common conception of bipolar disorder is that it’s a mental health condition with energetic and depressive episodes. While that’s partially true, it’s an oversimplification that misses the distinction between bipolar I and II. The differences between these two are important, since the treatment plan for each varies.
“Getting the right diagnosis matters,” says MaryEllen Eller, MD, regional medical director at Radial, “It changes the trajectory of treatment, the prognosis, how frequently we need to follow up, and what we need to do to manage the disease.”
Unless you’re a psychiatrist reading this, you won’t be diagnosing anyone with either type of bipolar disorder. But understanding bipolar disorder and its various types can empower you to have more informed conversations with your healthcare team or to better support a loved one with this condition.
What is bipolar disorder?
Put most simply, bipolar disorder is a mental health condition where a person alternates between episodes of depression and mania (with healthy periods in between). A person with bipolar disorder might also experience mixed episodes, with features of both depression and mania or hypomania, at the same time. These episodes mark dramatic shifts in mood and energy levels that interfere with daily life, and can last weeks at a time.
But while that definition explains the condition at the most basic level, it doesn't speak to the important nuance of the three types of bipolar disorder:
- Bipolar I: Bipolar I is marked by severe manic episodes. Many with this type also experience episodes of bipolar depression, though only manic episodes, not depressive episodes, are necessary for a bipolar I diagnosis.
- Bipolar disorder II: This bipolar disorder type is characterized by episodes of severe bipolar depression. Instead of full-blown mania episodes, those with this type experience less severe manic episodes (referred to as hypomania).
- Cyclothymia: The last of the common types of bipolar disorder is cyclothymia. With this type someone experiences episodes of hypomania and periods of low mood, though the depressive symptoms are not as severe as in bipolar I, bipolar II, or major depression.
All bipolar disorder types are relatively rare compared to conditions like major depressive disorder or generalized anxiety disorder. About 2.8% of adults in the US experienced a bipolar episode in the last year.
You may be wondering if the bipolar I and bipolar II distinctions mean one version is more severe than the other, but that’s not the case. Both types can be severe in their own ways. Of those with bipolar disorder I and II, 82.9% experienced serious, debilitating symptoms, underscoring the seriousness of this condition.

Bipolar disorder symptoms
It’s uncommon for symptoms to occur on an ongoing basis; usually they are seen in episodes of mania and/or depression.
Mania symptoms may include:
- Feelings of paranoia
- Intense irritability
- Extreme happiness or excitement
- Feeling restless or energetic
- Not requiring much sleep
- A racing mind
- Trouble concentrating
- Saying a lot and/or talking fast
- Feeling overly confident
- Higher than usual sex drive
- Uncharacteristic risk-taking and impulsivity
- Feeling overly confident
- Hearing or seeing things that aren’t there (hallucinations)
- Delusions or fixed, false beliefs
- Suicidal ideation
Depression symptoms may include:
- A continuous depressed mood
- Fatigue or low energy
- Disinterest in hobbies and social activities
- Trouble sleeping or sleeping too much
- Difficulty thinking or making decisions
- Negative thoughts about themselves and the world around them
- Trouble engaging in daily activities, like brushing teeth or making the bed
- Suicidal ideation
Between these episodes, people often experience return-to-normal periods referred to as euthymia. “In the time between episodes, people are highly functional,” says Dr. Eller, “They can have a normal mood, a normal job, family, all the things, but they have episodes where the disease can take over the way that they're thinking and can make them act very out of character for how they would if they did not have this disease.”
It's estimated that on average people with bipolar disorder spend about half of their life in a euthymic state. But of course this can vary greatly from one person to another. The aim of treatment for bipolar disorder is to minimize spells of depression and mania (or hypomania) and to make those euthymic periods last longer.
Key differences between bipolar 1 vs. bipolar 2
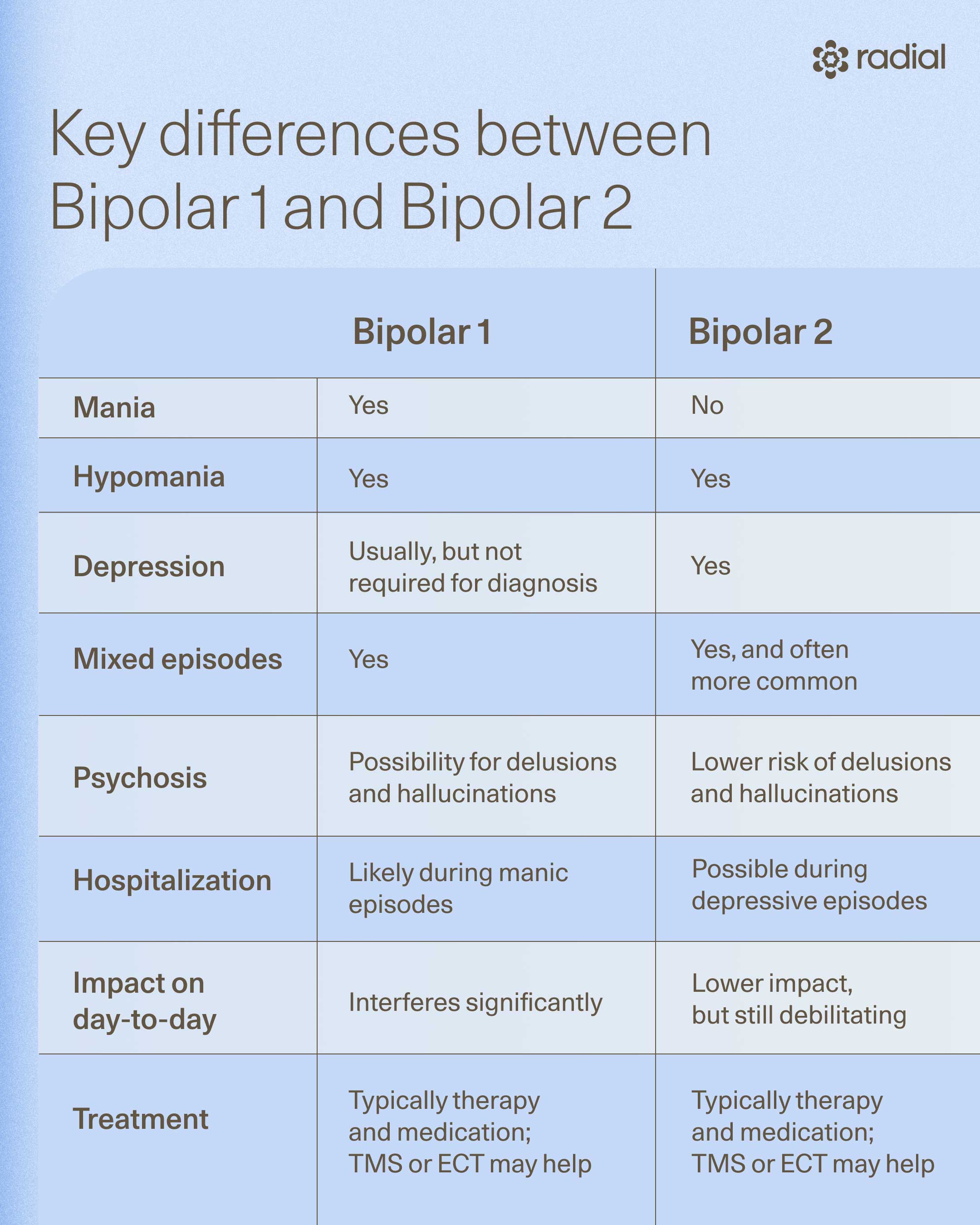
Mania vs. hypomania
If someone is over-the-moon happy for a week because they got a promotion at work or the weather is great, that’s not mania. It’s normal human behavior. Mania is something much more extreme that only occurs in bipolar disorder I. It’s marked by symptoms like talking fast, increased energy throughout the day, a decreased need for sleep, and extreme risk-taking.
“A manic episode is basically the brain getting stuck in a disease state of increased energy. That can be euphoria but that can also be feelings of irritability,” explains Dr. Eller, “If left untreated, mania ends in jail, hospitalization, or death.” By definition, these episodes last at least seven days. The one exception is if a mania episode results in someone being hospitalized before the seven day mark.
While half of people with any bipolar disorder experience symptoms of bipolar psychosis (hallucinations or delusions) at least once in their lifetime, it is more common in bipolar disorder I and usually occurs during manic episodes.
Hypomania is similar, but less extreme—and much more challenging to diagnose since people don’t typically seek psychiatric help for it. “Hypomania has a lot of the symptoms of mania, but with a much lower intensity that doesn't lead to functional impairment. So someone is not going to lose their job or get divorced because of hypomania,” says Dr. Eller.
This means those who experience hypomania aren’t going to take huge risks that end in life-altering events or time in the hospital or prison. They will, however, think quicker, have less self-doubt, and often be more productive than usual. Hypomania lasts at least four consecutive days and must be present for a majority of each day.
Depression in bipolar 1 vs. bipolar 2
Bipolar depression is as severe and debilitating as major depressive disorder (MDD). In fact, it shares all of the same symptoms and is often misdiagnosed as MDD. To be considered a bipolar depressive episode, the symptoms must last at least two weeks, and the period must be marked by an abrupt change in how an individual acts, not just feeling a little under the weather or melancholic.
The severity of depression and the length of depression spells in bipolar disorder might be more severe in bipolar disorder II than in bipolar disorder I. One study found that those with bipolar disorder II spent 40% more time in depressive episodes than those with bipolar I and had more difficulty recovering after an episode.
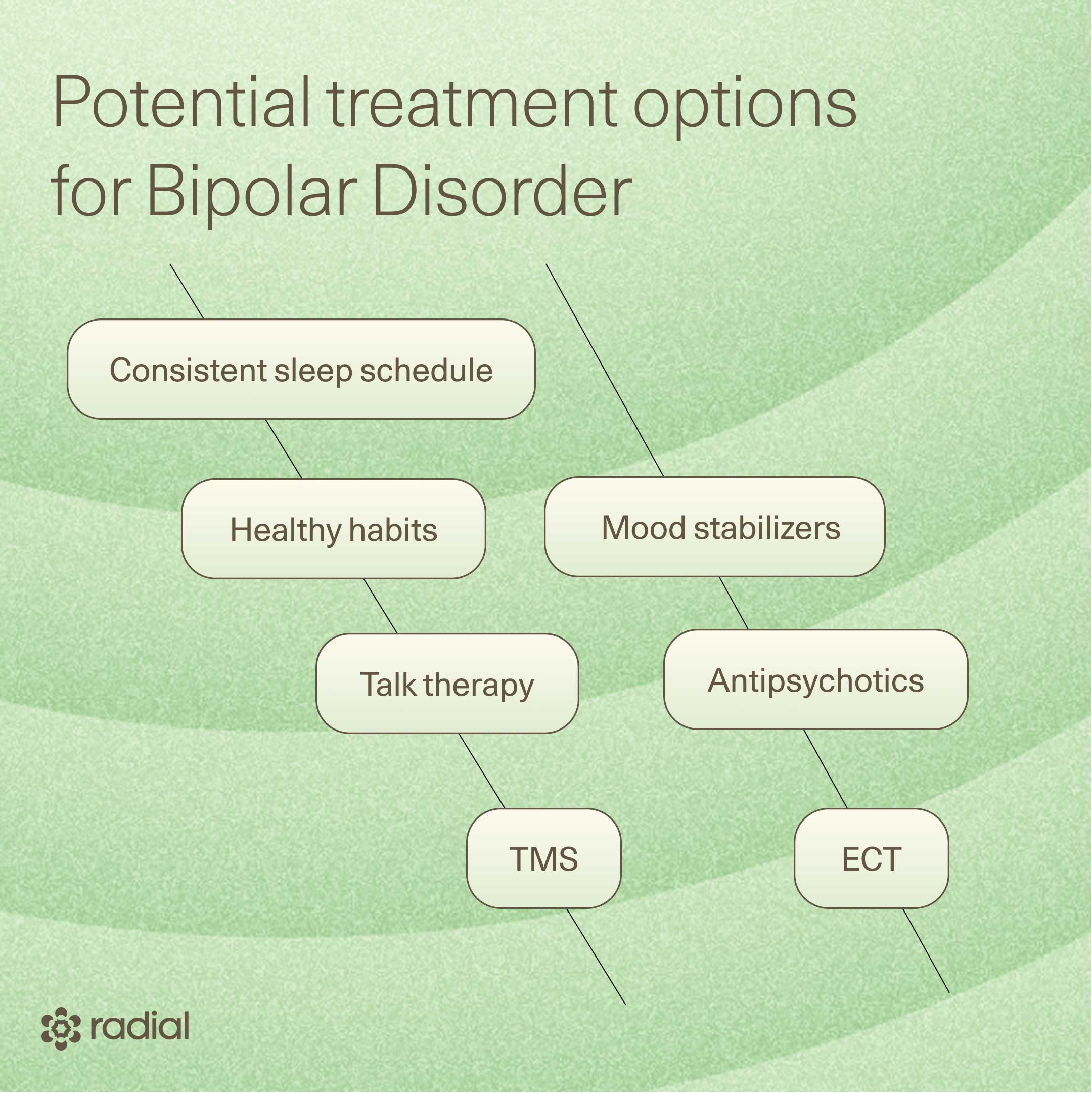
Treatments for bipolar 1 vs. bipolar 2
While bipolar disorder can’t be cured, many patients achieve recovery with effective treatment. The goal of treatment is to minimize mania and hypomania, and also to minimize depression. In order words, the goal is to maximize euthymia. Treatment for bipolar disorder usually consists of a mix of medications, device-based interventions, psychotherapy, and lifestyle changes. There are also some emerging bipolar disorder treatment options, particularly for bipolar II, that show promise.
Lifestyle habits
The advice to “develop healthy habits" is a cliche because it works. For bipolar disorder specifically, good habits lessen symptom severity during manic and depressive episodes and improve overall quality of life.
A 2023 review on lifestyle interventions for bipolar disorder revealed the most impactful habits are:
- Get consistent, quality sleep each night
- Eat a healthy, well-balanced diet
- Get regular physical activity, which could be an hour long strength training session or a walk around the block
- Limit (ideally stop or don’t start) the use of alcohol and recreational drugs
- Manage stress, which can be done through meditation, journaling, or other relaxing activities
- Maintain relationships with friends and family—people with bipolar disorder are more likely to experience severe episodes of bipolar depression if they feel lonely or disconnected from those around them
Medications
Mood stabilizers are the most common bipolar disorder medication. These are a class of medications that, for lack of a better term, sfor lack of a better term, tend to "stabilize" mood toward a euthymic state. In other words, they tend to prevent spells of mania, hypomania, and depression. “When we’re looking at bipolar depression, the mainstay medication that has the best efficacy is lithium,” says Dr. Eller. Other common mood stabilizers are lamotrigine (lamictal), divalproex (also called valproate or valproic acid), and carbamazepine.
“Lithium, of all medicines, is crucially important because it greatly reduces the risk of death by suicide,” says Owen Muir, MD, DFAACAP, an interventional psychiatrist and the co-founder and Chief Medical Officer of Radial, “given that 10-15% of people with bipolar disorder die by suicide, this is a huge deal.”
Antidepressants—medication classes that block reuptake pumps that clear mood-regulating transmitters in order to improve the way the brain regulates mood—have been prescribed as a bipolar 2 medication in the past. However, this is highly controversial since they increase the risk of manic episodes. They are no longer recommended for bipolar disorder because they are associated with more switches to mania than other medication classes.
“International consensus is that SSRIs, SNRIs, and other ‘unipolar antidepressants’ both don’t work and might increase risk in bipolar disorder of any kind,” notes Dr. Owen Scott Muir, M.D., DFAACAP a dual-board certified child and adult psychiatrist and CMO of Radial.
Additional bipolar 1 medications may be prescribed on an as-needed basis to target specific symptoms. When mania episodes make it difficult to sleep, for example, a psychiatrist may prescribe a sleep medication, like benzodiazepine or a sedative. An antipsychotic may also be prescribed, either as a maintenance drug or during mania episodes, since these medications reduce manic and psychosis symptoms.
Should insomnia or sleep difficulties be present in bipolar 2, a different sleep medication, such as Suvorexant, a hypnotic medication that makes someone sleepier at night. However, evidence is mixed if medication is the best route, and most psychiatrists steer patients toward lifestyle changes instead.
Interventional and emerging treatments
While many of the medications mentioned are effective, they come with some serious side effects. If used for years, lithium, for example, may cause metabolic disorder, thyroid issues, weight gain, and even interstitial nephropathy, an inflammatory kidney disorder that can lead to kidney failure. The side effects (especially the more severe ones) are rare, and can be prevented with proper monitoring from a qualified provider.
Still, researchers are actively searching for treatments with fewer side effects, and they’ve found a few options that are particularly effective for bipolar depression. A treatment for bipolar disorder II with fewer side effects but similar efficacy levels is transcranial magnetic stimulation (TMS).
TMS is a neuromodulation therapy where a noninvasive electromagnetic device, usually in the shape of a cap or paddle, delivers magnetic pulses that induce tiny electrical currents. These currents help fine-tune mood-related neurons, producing changes in how the brain operates.
When TMS targets specific circuits in the brain involved in bipolar depression, it greatly reduces depressive episode frequency and severity. However, it’s not FDA-cleared for bipolar depression specifically, meaning some insurance companies may not cover treatment costs.
Another option that is indicated for manic, depressive, and mixed episodes? Electroconvulsive therapy (ECT). “Traditionally, if medication didn't work, you had ECT as a failsafe for acute treatment of depression episodes or manic episodes,” explains Dr. Eller.
ECT delivers dosed electrical currents that change the neural pathways involved in manic and depressive episodes. A side effect is that it induces controlled seizures, which is where it gets its bad rep as “shock therapy.” In the past, caution was warranted, since patients underwent ECT without anesthesia, meaning they had to experience the seizures. Today, ECT is performed with anesthesia, making it a more safe, tolerable, and effective option.
Psychotherapies and supportive treatments
In addition to medication for bipolar disorder, a course of therapy is an important element of treatment. In fact, one study suggests that those with bipolar disorder who attend bipolar disorder supportive therapy sessions (alongside medication and other treatments) are 1.58 times as likely to remain clinically stable.
The most common types of therapy for bipolar disorder combine psychotherapy (talk therapy focused on someone’s thoughts, behaviors, and emotions) with psycho-skills development, which is therapy that builds skills to use when a bipolar episode strikes.
These can include:
- Cognitive behavioral therapy (CBT): Helps identify and reframe negative thought patterns and behaviors.
- Interpersonal and social rhythm therapy (IPSRT): A type of therapy specifically for bipolar disorder. IPSRT helps individuals manage stressful events, develop good social routines and a healthy circadian rhythm, and continue to take bipolar medications.
- Family-focused therapy: Intended for adolescents or kids with bipolar disorder and their families. Together, families work to develop better psychosocial functioning and learn how to address bipolar symptoms.
- Psychoeducation: When a therapist educates someone on their type of bipolar disorder, helps them to identify warning signs of an episode earlier, and offers strategies for better medication adherence.
Living with bipolar disorder
We can’t emphasize enough how severe bipolar depression and mania are. If left untreated, bipolar I and II can impact everyday life, lead to life-altering events, like divorce or being unable to hold down a job, and increase the risk of suicide and suicidal ideation. One study suggests 48% of men with bipolar disorder and 44% of women report suicidal ideation, and the attempt and suicide death rates are higher for those with this condition than the general population.
While those with bipolar I and II spend an average of about half of their life in euthymia, episodes of mania, hypomania, or depression can happen at any time. One study estimates that those with bipolar I average about 30% of the year in depressive episodes and 10% in mania. Those with bipolar II average depressive symptoms for over half of the time, and hypomanic symptoms a small (1.4%) amount of the time. Of course, these are just averages, and each person with bipolar disorder is unique and will often have a pattern quite different from the average.
Part of a robust treatment plan is understanding bipolar disorder episodes, what symptoms usually occur first for an individual, and having resources on hand for when episodes start. Those resources might include:
- A psychiatrist and support network of loved ones who can spot early symptoms
- Self-care strategies and routines that help stabilize mood
- Additional medications or treatments for when episodes occur
A psychiatrist can help you build out your bipolar episode toolkit, but know that successfully living with bipolar disorder involves consistent treatment and vigilance for early warning signs of episodes.
When and how to seek help
If experiencing any symptoms that may be due to bipolar disorder I or II, see a healthcare provider. Ideally, this should be a psychiatrist who has treated other patients with bipolar disorder. After a thorough evaluation and diagnosis, they can prescribe the right medications and treatments to manage symptoms, as well as provide bipolar disorder supportive therapy.
“As a physician who also lives with bipolar disorder, the most important thing to work out with your doctor, if you are worried about bipolar disorder, is if you have bipolar or unipolar illness. It’s more ‘obvious’ in bipolar I, but no less destructive to your quality of life to have bipolar II, and both are serious medical conditions,” notes Dr. Muir.
If unsure where to find a psychiatrist, you can either contact a psychiatric practice with experience treating bipolar disorder, like Radial, or utilize the psychiatrist directories on the CDC’s website.
Should you experience suicidal ideations or other extreme symptoms, don’t wait for a psychiatry appointment to get help. If you’re in a crisis or considering suicide, call or text 988 or visit their website.
The bottom line
Bipolar disorder I and II are both serious, life-altering conditions. While neither has a cure, the right treatment can prolong the time between episodes and decrease symptom severity. Working with a psychiatrist who is familiar with both types of bipolar disorder, such as the team at Radial, is essential for an accurate diagnosis and an effective, sustainable treatment plan.
Key takeaways
- Bipolar disorder I is marked by manic episodes lasting longer than seven days. Most people with this type of bipolar disorder also experience depressive episodes, though this isn’t essential for diagnosis.
- Depressive episodes are an essential component of bipolar disorder II. People with this condition also experience periods of hypomania, a less severe form of mania.
- For bipolar I and II, it’s important to get an accurate diagnosis and appropriate treatment plan. With the right medications, therapeutic approaches, and lifestyle interventions, it’s possible to extend the time between episodes, reduce episode severity, and live most of life in a calm and regulated state.
Frequently asked questions (FAQs)
What is the difference between type 1 and type 2 bipolar disorder?
The difference between bipolar disorder I and II is the type of episodes someone experiences. With untreated bipolar I, one experiences episodes of mania that last at least seven days or end in hospitalization before the seven day mark. One may also experience episodes of bipolar depression, though these aren’t necessary for a bipolar I diagnosis.
On the other hand, depressive episodes are a diagnostic criteria for bipolar II, which is often misdiagnosed as major depressive disorder (MDD). Someone with bipolar II also experiences hypomania episodes, which are similar but less severe than mania episodes.
Is bipolar I of II more serious?
Neither is necessarily more severe than the other. Both negatively impact everyday life, increase the risk for suicide, and can impair one’s ability to function at work and in their social life.
How many types of bipolar disorder are there?
There are three common types of bipolar disorder. Bipolar disorder I is marked by episodes of mania that last at least seven days, unless hospitalized before the seven-day mark. Someone with bipolar I may also experience depressive episodes, though these aren’t required for diagnosis. Bipolar disorder II consists of episodes of depression and hypomania, a less severe form of mania. The third type, cyclothymia, consists of similar hypomania symptoms as bipolar disorder II and less severe depressive episodes. And also, on average the depression is often more debilitating with bipolar II.
Can you have both bipolar I and II?
You cannot have bipolar I and II simultaneously because mania is an essential feature of bipolar I and must be absent to be diagnosed with bipolar II. In other words, if someone has a spell of mania then going forward we call their condition bipolar I, and not bipolar II. However, it is possible to have both at different points in your life since bipolar disorder occurs on a spectrum, and someone can experience symptoms at multiple points on that spectrum during their lifetime.
Deep dive recommendations:
- The Frontier Psychiatrists. An Open Letter to My Bipolar Disorder.
- Before You Kill Yourself: A Suicide Prevention Podcast. Bipolar: How to Feel Understood and Why You End Your Sentences With Question Marks.
- OurView Podcast. Bipolar Disorder: A Conversation with Dr. Owen Muir.
- The Frontier Psychiatrists. How to Survive Bipolar Disorder.
- The Frontier Psychiatrists. Does Lithium Prevent Suicide in Bipolar Disorder? An Existential Guide.
- Ellen Frank. Treating Bipolar Disorder: A Clinician's Guide to Interpersonal and Social Rhythm Therapy (Guides to Individualized Evidence-Based Treatment).
- Julie A. Fast. Loving Someone with Bipolar Disorder: Understanding and Helping Your Partner (The New Harbinger Loving Someone Series).
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started



