What Is Postpartum Anxiety? Signs, Causes, and Treatments
.jpg)
If you’ve spent nights wide awake, heart pounding, convinced something’s wrong with your baby (or yourself), you’re not alone. Postpartum anxiety can make even calm moments feel like alarms are going off inside your body. It’s more than “new mom worry”—postpartum anxiety is a real, common, and treatable condition that affects millions of new parents each year. And while it can feel like you’re the only one on edge when everyone else seems to be adjusting, you’re not broken—you’re human, and there are treatments to help.
After having a baby, some worry is expected. You might double- (okay, triple-) check the monitor at night or feel uneasy the first time you leave your child with someone else. But if those worries don’t fade with time, it’s more than new-parent nerves: It’s postpartum anxiety.
Postpartum anxiety affects an estimated one in four women, though experts believe it’s underdiagnosed because symptoms often get brushed off as stress or labeled as postpartum depression.
“Unlike passing worries, postpartum anxiety can involve constant fear, physical symptoms like a racing heart or shakiness, and unwanted, intrusive thoughts that are hard to ignore,” says Greg Malzberg, MD, a psychiatrist at Radial, and editor of the PsychoPharm Podcast.
In this guide, we’ll unpack what postpartum anxiety is, how it differs from depression, and the most effective treatment options. Most importantly, you’ll learn that recovering from postpartum anxiety is entirely possible.
What is postpartum anxiety and how is it different from typical new-parent worries?
Feeling on edge after having a baby is normal—after all, your world just changed overnight. Postpartum anxiety (or PPA postpartum) is different. The worry doesn’t turn off; it ramps up. Many parents describe it as a sense of dread they can’t explain or a feeling that something bad is always about to happen.
In clinical terms, postpartum anxiety is an anxiety disorder that develops during pregnancy or within the first year after childbirth. It can trigger physical symptoms like:
- restlessness
- heart palpitations
- nausea
- irrational thoughts
- social avoidance
- need for control
“Because exhaustion is so common after birth, postpartum anxiety can sometimes be overlooked. One helpful distinction is how much symptoms interfere with daily life,” says Sarah Quaratella, MD, a psychiatrist at Hartselle & Associates. “With postpartum anxiety, anxiety begins to affect functioning, making it hard to relax, enjoy time with the baby, or even leave the house. In contrast, typical new-parent worries tend to come and go, ease with reassurance, or improve with rest.”
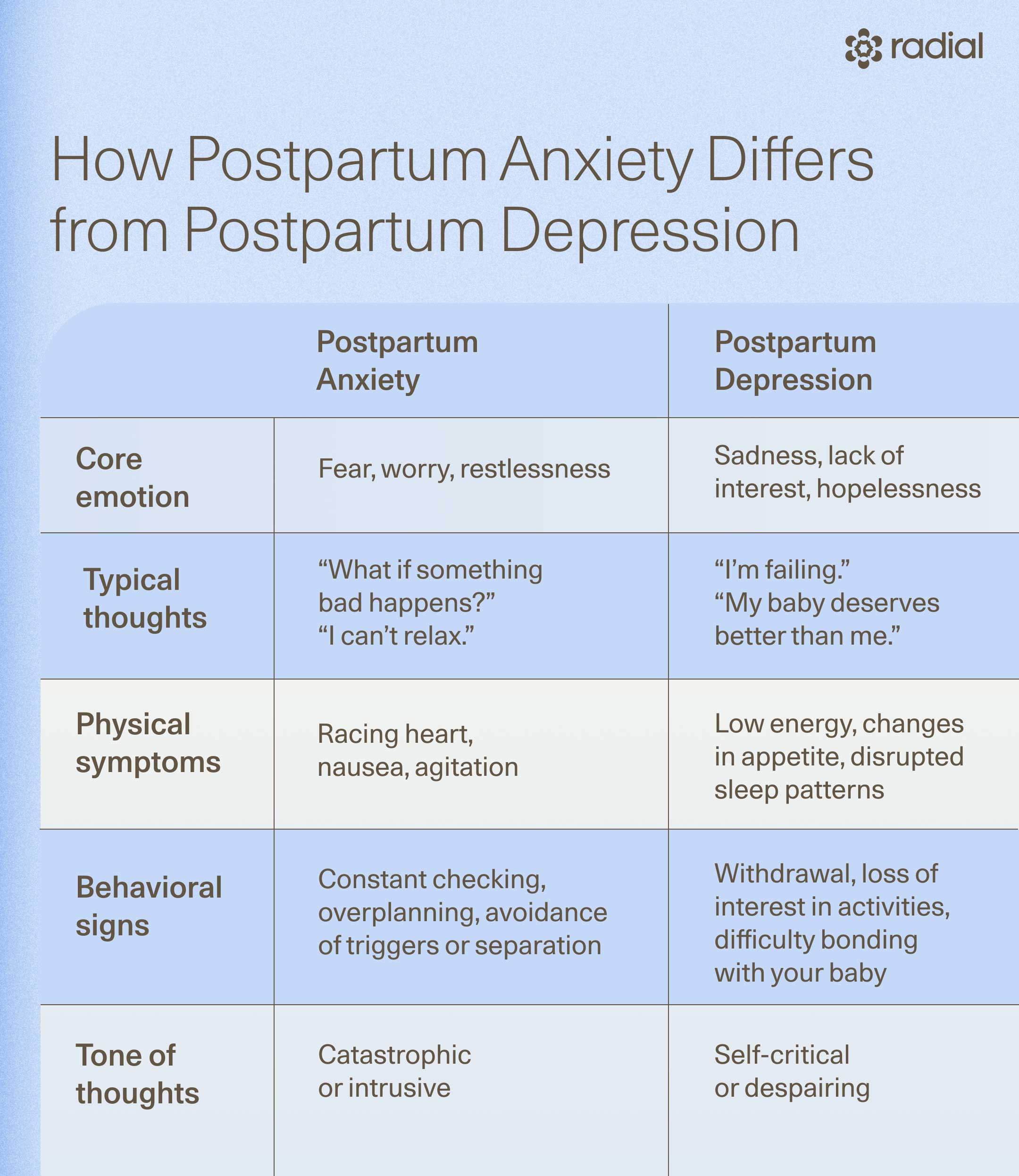
How is postpartum anxiety different from postpartum depression?
While postpartum depression and anxiety often overlap—and can even occur together—they affect thoughts, emotions, and behaviors in different ways.
“A mother with anxiety may feel constantly alert and unable to relax, while someone with depression may feel numb or disengaged,” says Malzberg. “Many women experience both conditions at the same time, which can make diagnosis more complex.”
Regardless, both conditions deserve attention and care. Here’s how they compare:
What is postpartum OCD?
For some parents, anxiety after birth shows up as intrusive thoughts. These are unwanted, often distressing mental images or fears, such as harm coming to the baby or accidentally doing something wrong. These thoughts are not desires or intentions; they’re anxiety’s way of trying to protect you by imagining worst-case scenarios.
When these intrusive thoughts lead to repetitive behaviors (like checking the baby’s breathing over and over, or avoiding sharp objects out of fear) or symptoms interfere with a normal mother-child relationship, clinicians may diagnose postpartum OCD.
It’s crucial to know this is not postpartum psychosis, which involves delusions or a break from reality and requires emergency care. People with postpartum OCD most often know their thoughts are irrational and feel horrified by them, but can’t stop those thoughts. It is possible for postpartum OCD to “tip over” the line into psychosis in extreme cases, and this would also be considered a medical emergency..
What are postpartum anxiety symptoms?
Postpartum anxiety can look and feel different for everyone. For some, it’s a constant hum of unease; for others, it’s waves of panic that come out of nowhere. Because anxiety affects both the body and the mind, its symptoms often show up across several domains, including physical, emotional, and behavioral.
Knowing what to look for can help you recognize when what you’re feeling goes beyond typical new-parent stress and may signal something more.
Physical symptoms
Anxiety doesn’t just live in your head—it’s a full-body experience, says Malzberg. Many new parents notice sensations that mimic medical issues, which can make the anxiety itself worse.
Common physical signs of postpartum anxiety include:
- Racing heart or palpitations that feel like panic or an impending medical emergency
- Shortness of breath or tightness in the chest
- Postpartum nausea or upset stomach that doesn’t have a clear cause
- Dizziness, trembling, or sweating even at rest
- Numbness and tingling
- Trouble sleeping, even when the baby is asleep and you’re exhausted
- Loss of appetite or difficulty eating due to constant tension
- Muscle tension, headaches, or fatigue from being in a prolonged state of alert
Emotional symptoms
Emotionally, postpartum anxiety often shows up as fear, guilt, or relentless “what if” thinking. It goes beyond general worry: it’s worry that is all-consuming. You might notice:
- Racing or looping thoughts about your baby’s safety or your ability to care for them
- Persistent dread or fear that something bad is about to happen
- Irritability or restlessness, especially when you can’t identify a clear reason
- Intrusive thoughts postpartum, often about harm coming to the baby or yourself (which can be extremely distressing, but do not mean you’ll act on them)
- Overwhelm or difficulty relaxing, even when everything seems okay
- Difficulty concentrating
- Difficulty making decisions
- Feelings of self-blame
Behavioral symptoms
Because anxiety activates the body’s fight-or-flight system, it can also drive behaviors that keep the cycle going. You might find yourself:
- Compulsively checking the baby’s breathing, temperature, or positioning
- Avoiding certain activities, like driving, sleeping, or leaving the baby with others
- Overplanning or overcontrolling daily routines to prevent imagined risks
- Constantly seeking reassurance from partners, friends, or online groups, but never feeling fully relieved
- Withdrawing socially, especially if you fear judgment or don’t want others to “see you like this”
These symptoms of anxiety can ebb and flow throughout the day but often intensify at night, when fatigue, isolation, and quiet amplify anxious thoughts.

What causes postpartum anxiety?
There’s no single reason postpartum anxiety develops, and that’s part of why it’s so often misunderstood. For most people, it’s a mix of biology, sleep deprivation, life changes, and emotional strain that together push an already-taxed nervous system past its limits.
“It usually develops from a mix of biological, psychological, and environmental factors,” says Malzberg. “Hormonal shifts after childbirth, sleep deprivation, and physical recovery can all affect emotional regulation.”
Here’s what’s typically at play.
Biological changes
After birth, levels of estrogen and progesterone plummet, says Quaratella. These hormones influence brain chemicals like serotonin and GABA, which help regulate mood and calm. At the same time, the body’s stress-response system (the HPA axis) is adjusting to new demands. Together, these rapid changes can make some people more vulnerable to anxiety in the postpartum period.
At the same time, surges in oxytocin and cortisol (the bonding and stress hormones) can make your system more alert, amplifying any preexisting anxious tendencies.
If you’re also dealing with thyroid issues, iron deficiency, or hormonal sensitivity, the physical component of anxiety can feel especially strong, showing up as jitteriness, nausea, or even heart palpitations.
Psychological factors
Pregnancy, birth, and new parenthood can stir up unresolved fears, perfectionism, trauma, or even postpartum rage. People with a personal or family history of anxiety, mood disorders, OCD, or trauma are also at higher risk—in fact, research suggests that their brains’ “alarm system” may be quicker to activate.
“Personality traits such as perfectionism or a strong need for control can also make someone more vulnerable,” adds Malzberg.
Social and environmental stressors
Even in the best circumstances, new parenthood can feel isolating. But when support is limited—or expectations are unrealistic—postpartum stress can build quickly.
According to Malzberg, contributing factors often include:
- Sleep deprivation, which impairs emotional regulation and heightens fear responses
- Lack of practical or emotional support, especially for single parents or those without nearby family
- Birth trauma or medical complications that make the postpartum period feel unsafe
- Major life transitions, such as moving, relationship strain, or returning to work early
- Cultural expectations that glorify resilience while minimizing real mental health needs
Who is most at risk?
Anyone can develop postpartum anxiety, but certain factors increase vulnerability, including:
- Personal or family history of anxiety, depression, OCD, or eating disorders
- Difficult or traumatic birth experience
- High-stress personality traits (like perfectionism or overcontrol)
- Lack of sleep or social support
- History of miscarriage, infertility, or loss
The good news: none of these factors mean postpartum anxiety is inevitable or untreatable. They simply highlight how much stress the body and brain absorb during this life shift and how crucial support and treatment can be.
How is postpartum anxiety diagnosed?
Postpartum anxiety often goes unrecognized because its symptoms overlap with what many people assume is “normal” new-parent stress, it’s easy to dismiss or minimize what’s happening. But if your worry feels constant or unmanageable, that’s not a personal failing—it’s a sign your body and brain need support, not judgment.
There’s no single test for postpartum anxiety, but providers use a mix of screening tools, rating scales, and conversation to understand what’s going on. Common tools include:
- Generalized Anxiety Disorder-7 (GAD-7): This clinical questionnaire measures how often you experience symptoms like restlessness, tension, or excessive worry.
- Edinburgh Postnatal Depression Scale (EPDS): A questionnaire that screens for postpartum mood disorders; certain questions can help flag anxiety.
- Yale-Brown Obsessive Compulsive Scale (Y-BOCS): Helps identify obsessive thoughts or repetitive behaviors linked to postpartum OCD.
What does postpartum anxiety treatment look like?
“Care often involves therapy, medication when indicated, and practical lifestyle support,” says Quaratella.
Because everyone’s experience is unique, providers often tailor these treatments to fit each person’s symptoms, adds Malzberg.
Here’s the breakdown of common and effective options that may be combined or used individually to find relief.
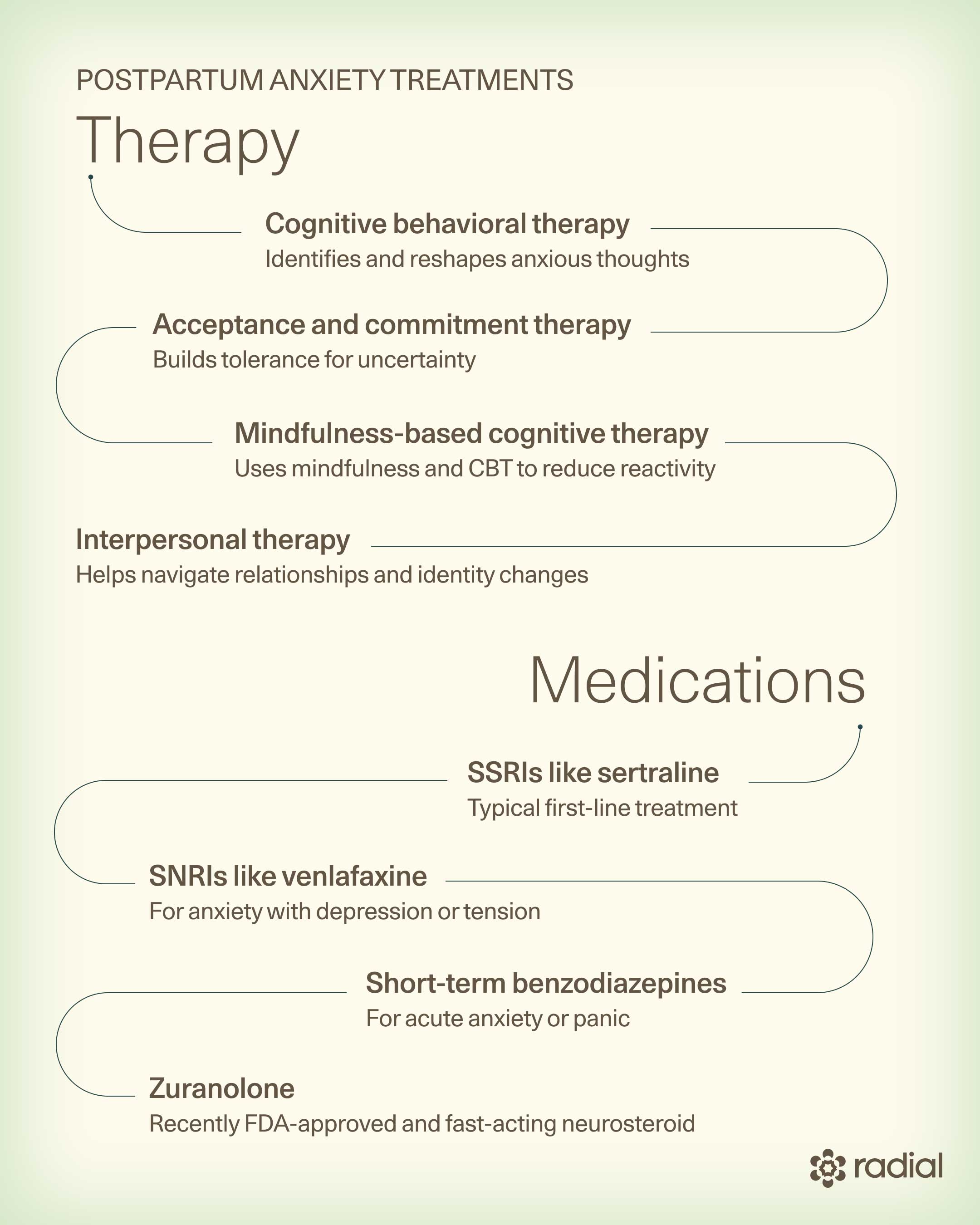
Therapy for postpartum anxiety
The first-line treatment is usually therapy, especially approaches that target anxious thought patterns and coping skills. Effective options include:
- Cognitive behavioral therapy (CBT): This approach helps parents recognize anxious thought patterns and replace them with more balanced, realistic ones.
- Acceptance and commitment therapy (ACT): This method builds tolerance for uncertainty and helps parents act in alignment with their values, even when anxiety is present.
- Mindfulness-based cognitive therapy (MBCT): This approach combines mindfulness practices with CBT techniques to calm the nervous system and reduce emotional reactivity.
- Interpersonal therapy (IPT): This type of therapy helps parents navigate relationship changes and evolving identity challenges in the postpartum period.
Medication for postpartum anxiety
If symptoms are persistent or severe—or if therapy alone isn’t enough—your provider might recommend postpartum anxiety medication, says Quaratella, including:
- SSRIs (like sertraline or escitalopram): These medications are well-studied in postpartum populations and are typically considered the first-line treatment for anxiety.
- SNRIs (like venlafaxine or duloxetine): These medications are especially useful when anxiety occurs alongside depression or physical tension.
- Short-term benzodiazepines: These medications may be prescribed under careful supervision to manage acute anxiety or panic attacks.
- Zuranolone: This is a recently FDA-approved, fast-acting neurosteroid that’s used to treat postpartum depression. It may also help with anxiety-related symptoms.
For breastfeeding parents, certain SSRIs and SNRIs (particularly sertraline) are generally considered safe. “Working with a provider who has experience in reproductive or perinatal psychiatry can be especially helpful, as they understand the unique considerations involved in medication management in the postpartum period,” says Quaratella.
Neuromodulation and interventional treatments
When anxiety doesn’t respond fully to therapy or medication or when parents prefer a non-drug option, interventional treatments like transcranial magnetic stimulation (TMS) can help.
TMS therapy uses gentle magnetic pulses to rebalance activity in brain regions involved in mood and anxiety regulation. It’s noninvasive, doesn’t require anesthesia, and is safe for breastfeeding parents. Many people report improvements in focus, calm, and emotional resilience within weeks. In a recent large-scale review, TMS was found to be very effective.
Lifestyle and social support
Supportive care is an essential part of recovery. Strengthening your body and your support system can help calm your mind, reduce the intensity of anxious thoughts, and make it easier to cope day to day. But for many people with postpartum anxiety, “just accept help” isn’t realistic—especially when your mind is telling you that only you can keep the baby safe.
Fortunately, “there are several skills and strategies that can be effective in managing anxiety for new mothers—which, by the way, is completely normal,” says Paige Bellenbaum, LCSW, PMH-C, a perinatal mental health specialist at Paige Bellenbaum Consulting.
Learning practical skills to manage anxiety in the moment can make sharing the load easier over time. Here are several approaches that Bellenbaum says can help:
- Counter catastrophic thinking: Identify your specific worry, then name the worst-case scenario, three other possible outcomes, and finally the most likely outcome.
- 4–7–8 grounding technique: Inhale through your nose for 4 seconds, hold for 7, and exhale through your mouth for 8. Repeat until your body starts to settle.
- 5–4–3–2–1 grounding technique: Look around and identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste to bring yourself back to the present moment.
- Building trust with other caregivers: Start with “bite-sized exposure.” Leave the baby for short, manageable intervals—a walk around the block, a quick coffee run, a brief errand—and gradually increase the time as your comfort grows. This incremental exposure helps rebuild trust and reduces separation-related anxiety.
“Remember, this is really hard for everyone. You are not doing anything wrong if you cry the whole time on that walk, while a part of you feels relief in having a minute to yourself,” says Bellenbaum. “In motherhood, there is always a both/and—both can be true at the same time. Learning to embrace the ambivalence is one of the ingredients that make you a great mom.”
There are also broader lifestyle habits that can support recovery:
- Sleep, nutrition, and hydration: Rest whenever possible, even in short bursts, and accept help with feedings or chores.
- Movement: Gentle activity like walking, stretching, or postpartum yoga can lower cortisol and regulate your nervous system.
- Peer support: Joining a group through Postpartum Support International or a local therapist can normalize what you’re feeling and reduce isolation.
- Partner and family communication: Sharing how anxiety shows up for you and asking for concrete help can prevent misunderstanding and burnout.
When and how to seek help for postpartum anxiety
You don’t need to hit a breaking point to ask for help. The right time to reach out is as soon as anxiety starts interfering with rest, connection, or daily life.
“It’s important to reach out for help if anxiety feels constant or overwhelming, if you’re unable to sleep even when you have the chance to rest, or if your worries are making it hard to function day to day,” says Quaratella. “If you’re unsure whether your symptoms are typical or part of postpartum anxiety, a trained mental health professional can help clarify and guide next steps.”
Consider reaching out to your OB-GYN, primary care provider, or a perinatal mental health specialist if you notice:
- Worry or panic that feels constant or unmanageable
- Physical symptoms like heart palpitations, shaking, or postpartum panic attacks
- Trouble sleeping even when the baby is asleep
- Intrusive thoughts that distress you or make you avoid certain activities
- A sense of dread, guilt, or disconnection from your baby or yourself
During an evaluation, your provider may ask about your symptoms, sleep patterns, and daily functioning, review medications or health changes, and use screening questionnaires to assess severity. They’ll also discuss treatment options.
If anxiety ever escalates to thoughts of self-harm or feeling that your baby would be better off without you, seek immediate help by calling the National Suicide Prevention Hotline (just dial 988) or going to the nearest emergency department. Postpartum Support International also offers free, confidential help and can connect you with providers with experience treating perinatal mental health conditions, adds Quaratella.
How to help someone with postpartum anxiety
Partners, family, and friends can make an enormous difference in recovery. Here’s how to show up in ways that truly help:
- Listen before you fix: Validate their feelings (“That sounds really hard.”) instead of jumping to advise.
- Offer practical help: Handle a feeding, household task, or errand so they can rest.
- Encourage treatment, not endurance: Remind them that help is available and effective. Offer to make the call or attend an appointment with them.
- Stay patient: Recovery takes time, and reassurance may need repeating.
- Avoid minimizing: Don’t say “all new parents worry” or “it’s just hormones.” Anxiety this intense isn’t “just” anything—it’s real, and it deserves care.
The bottom line
Postpartum anxiety can feel isolating, but it’s far more common than most people realize, and it’s not a reflection of how strong or loving you are as a parent. Instead, it’s your body’s way of signaling it needs support after a major physical and emotional shift. With the right care—whether therapy, medication, TMS, lifestyle changes, or a mix of treatments—relief is possible, and recovery is the rule, not the exception.
Key takeaways
- Postpartum anxiety is common and treatable. It affects about one in four new parents and can appear anytime in the first year after birth.
- It’s more than “normal worry.” The anxiety feels constant, overwhelming, and often comes with physical symptoms like nausea, heart palpitations, or panic attacks.
- Intrusive thoughts are common. They’re distressing but do not reflect intent or character.
- Therapy, medication, and newer options like TMS therapy can all help regulate your nervous system and restore calm.
- Early help makes recovery smoother. The sooner you reach out to a healthcare provider or perinatal therapist, the faster you can start feeling like yourself again.
Frequently asked questions (FAQs)
How long does postpartum anxiety last?
The duration varies for everyone. Some people feel better within weeks of starting treatment, while others notice gradual improvement over several months. Without support, symptoms can persist for years. But with treatment, medication, and lifestyle changes, most parents recover fully within the first year.
What does postpartum anxiety feel like?
Postpartum anxiety can feel like your mind and body are on high alert. You might have racing thoughts, a pounding heart, or an unshakable sense that something bad could happen. Many parents describe it as being “stuck in fight-or-flight mode”—exhausted but unable to relax, even when everything seems fine.
Can postpartum anxiety go away on its own?
Sometimes mild symptoms improve with rest and support, but most people benefit from professional help. Treatment shortens recovery time, prevents anxiety from deepening, and makes coping easier day to day. Reaching out for care isn’t a sign of weakness: It’s an act of protection and care for both you and your baby.
Deep dive recommendations
- Psychiatry and Psychotherapy Podcast. Episode 033: Perinatal Mood and Anxiety Disorders. https://www.psychiatrypodcast.com/psychiatry-psychotherapy-podcast/2018/11/14/perinatal-mood-and-anxiety-disorders?rq=postpartum
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




