Depression Success Stories: What Recovery Looks Like
.png)
Living with depression can feel isolating and heavy at times, but it’s important to remember you’re not alone and that healing is possible. Sometimes, finding the right support and treatment just takes a bit of time. Our wish is that the following depression success stories may provide hope and inspiration, as well as potential treatments to explore.
Depression can make it difficult to get out of bed in the morning, much less find the energy to invest in overcoming it. But even during the most intense episodes, there is hope. These depression success stories document how others were able to beat the fog and heaviness of this mental health condition. Afterwards, these patients built lives full of joy, reconnected with their passions and loved ones, and discovered who they were outside of depression.
With the right treatments and provider, beating depression is possible, even in cases where talk therapy or antidepressants didn’t work on their own. Ahead are five real stories of overcoming depression from individuals who once doubted if recovery was possible, only to discover that it was.
Healing after treatment-resistant depression: Tara’s story
At least 30-50% of people with major depressive disorder (MDD) live with treatment resistant depression, a condition that is diagnosed when MDD doesn’t improve with talk therapy or conventional medications alone. Transcranial magnetic stimulation (TMS) is one of the most effective treatments for medication- and therapy-resistant depression, as Tara Duncan knows all too well.
TMS is a FDA-cleared, non-invasive treatment where an electromagnetic coil is placed near the scalp. This coil sends magnetic pulses to certain areas of the brain, strengthening healthy neural connections to help people overcome many conditions, including MDD. Almost 60-80% of people experience remission with accelerated TMS, the most effective version of this therapy.
Despite its success, many people don’t know about this treatment. Tara, for example, only found out about TMS when her provider recommended it.
Before getting insurance approval for TMS treatment, she tried over nine medications for her major depressive disorder with distressing suicidal thoughts. As Tara continued with medication, the dosages became higher, and she was eventually on the highest dose of two medications. While they worked, she worried about what would happen once her body adjusted to the highest doses. That’s when she and her provider advocated for TMS with her insurance company, which she noted was an uphill battle.
“After a year, nine different meds, plenty of therapy, and still maybe only 80% back to myself, my insurance finally approved TMS,” says Duncan, “TMS can be uncomfortable, and it’s a gradual improvement. You kind of just wake up one day and realize your brain has been quieter or you haven’t thought about ending it in a while.”
Two years later, Tara’s thoughts of self-harm have disappeared, and her depression is in remission. She’s only on a half-dose of one medication, not multiple, in order to maintain TMS progress. “I am having appropriate emotional responses to difficult things, I enjoy life more, and I’m more positive,” reflects Duncan, “I highly recommend TMS!”
Depression and chronic conditions: Browne’s story
Browne Smith has been living with treatment resistant depression for over 30 years. She had tried prescription medications and St. John’s Wort, but the side effects from both were difficult to manage.
Browne also lives with fibromyalgia, rheumatoid arthritis and Ehlers-Danlos syndrome, conditions that often co-occur with depression. Chronic physical illnesses can contribute to emotional distress, while depression can worsen physical symptoms, creating a challenging cycle to manage.
When scrolling Instagram in 2024, Smith came across a post from Radial describing treatment options she had yet to try. Since then, she’s made leaps and bounds in her mental health journey and avoided the side effects of the treatments she previously tried.
“Since becoming a patient of Radial, and of Dr. Muir’s, I am changing my life for the better,” says Browne. “I am going to physical therapy now. I am exploring new ways to cope with my depression and other diseases.”
Now, Browne manages her depression through a combination of talk therapy, which she has used for years, and a new-to-her treatment, Prism neurofeedback therapy. In this form of brain training, the participant wears a cap with electrodes that monitor brainwave activity. The system translates these signals into audio and visual feedback, which is displayed on a screen. This real-time feedback helps the brain learn to self-regulate thoughts and feelings, offering an improvement rate of 78% for those with major depressive disorder.
While Browne is only halfway through this treatment, she is already finding many benefits for her depression. She also hasn’t experienced any side effects with Prism, a welcome reprieve after St. John’s Wort and medication. Prism sessions, she notes, are even kind of fun.
Smith also continued talk therapy, which she has found helpful throughout her journey with depression. “I would recommend talk therapy for anyone who has depression, no matter what other treatments they are using,” says Browne. “It’s literally kept me alive and made my life better than without it. It’s an outlet like no other to help me understand what is really going on with me, my depression, and other disabilities.”

Depression and OCD: Ari’s story
While Ari Trette has struggled with obsessive-compulsive disorder (OCD) her entire life, the COVID-19 pandemic made it unmanageable and severe. Ari’s experience reflects a broad trend: The World Health Organization reported that anxiety and depression rose 25% in the years following the COVID-19 pandemic.
For Ari specifically, anxiety manifested as a severe fear of contamination, a condition marked by intense obsessions about dirt or disease and compulsive cleaning behaviors. She also began struggling with intense sadness, worry, and isolation that eventually led to a diagnosis of major depressive disorder.
Since then, Ari has tried six different types of therapy, ten psychiatric medications, and two intensive treatment programs, all of which brought short-lived success. Eventually, she found exposure response prevention, a psychotherapy for OCD where you’re gradually exposed to your fears or obsessions, and TMS. Together, the treatments helped with managing depression and OCD.
TMS in particular moved the needle for her depression. “TMS became one of the best decisions I ever made for my mental health,” says Ari, who opened up about her journey on social media. Since then, she’s had tons of questions about the procedure, particularly about what it feels like and if it’s painful.
At first, TMS felt very strange to Ari, almost like being poked. After a few minutes, she stopped noticing it, and her care team found ways to make her comfortable throughout treatment.
Ari also appreciated that she could track her progress. Before TMS sessions, she filled out a questionnaire about her depression and OCD symptoms. “Slowly but surely, I began to notice it had been longer and longer since feeling depressed,” says Ari. “My OCD had gotten easier to manage, and I was finally living my life.”
Today, Trette feels lighter, almost as if a weight had been lifted from her shoulders, and like she can finally see clearly again. She’s returned to hobbies she used to love, such as painting, sewing, and embroidery, started rock climbing, reconnected with old friends, and made new ones.
“So much of my world was plagued by my depression and OCD. It’s been the first time in what feels like an eternity that I am truly living,” explains Ari. “I have discovered who I am without mental illness taking over my life. It’s amazing!”

Hope after years fighting depression: Stephanie’s story
Living with depression when your loved ones don’t “get it” often makes recovering from severe depression more difficult. Stephanie Forlini understands the isolation this condition can cause, which is part of why she started documenting her journey with depression on her social media.
Over the years, she’s tried so many SSRIs and SNRIs that she has lost count. Some helped temporarily, others not at all, and most came with heinous side effects. “Nothing really worked and I felt like I exhausted my options, until I found TMS,” says Forlini.
Forlini is still receiving TMS sessions; she was surprised to discover that the actual sessions only last about three minutes, with the setup taking longer than the treatment itself. She appreciates the encouragement from her care team and social media community throughout her journey — both are welcome reminders of the support she has in beating depression.
“I am about one fourth of the way done, but I have already noticed results,” says Forlini, “My depression score went down 7 points on the PHQ9 within 7 sessions of TMS. I am hopeful that the results will continue at this rate and am looking forward to the possibility of remission, like so many others who have done this treatment.”
From no motivation to marathon training: Kristen’s story
Two and a half years ago, Kristen M. Gingrich, LCSW, CADC, CCS, a licensed therapist and mental health content creator, could barely get out of bed and found everyday tasks hard to accomplish. Now, she’s waking up at 5am to run 18 miles as she trains for her first marathon. What exactly changed during that time? She found a way to recover from major depressive disorder.
Kristen has been living with major depressive disorder since she was 16. In that time, she tried multiple antidepressants, but none fully worked. At 31, she finally discovered TMS. Even with TMS, her depression didn’t disappear on day one.
Luckily, her provider set her up with realistic expectations, reminding her that progress would happen slowly over the course of the sessions. By session 11, she woke up feeling lighter, almost as if she had been carrying 10 stones the day before and now only had nine.
“I remember sitting there in that moment saying, if this is all that happens, this is all the relief I get, I'm okay with it,” says Kristen. Even that small change made it easier to get out of bed, brush her teeth, and shower.
By session 28, the intensity of Kristen’s depression symptoms became less severe, and continued to lessen through the end of treatment and after. It’s been two years since her initial round of TMS, and she still experiences a level of motivation and a lightness she hadn’t felt living with depression.
But TMS wasn’t the only treatment she found useful. Kristen received talk therapy before, during, and after her TMS treatments. She also stayed on her antidepressant throughout treatment and in the six months after, but has since stopped her medication. After treatment, the role of talk therapy shifted to helping her discover who she was without the depression.
“Talk therapy was really great to have after [TMS] because I had to get to know myself outside of depression,” says Kristen. “I've had depression probably since I was 16, if not before. I only knew myself as depressed. When that veil is taken off, you have to figure out who you are outside of that.”
The treatment paths that helped relieve depression
There isn’t a one-size-fits-all approach for depression. Instead, many potential treatments that may help, including talk therapy, TMS, PRISM neurofeedback, and lifestyle changes.
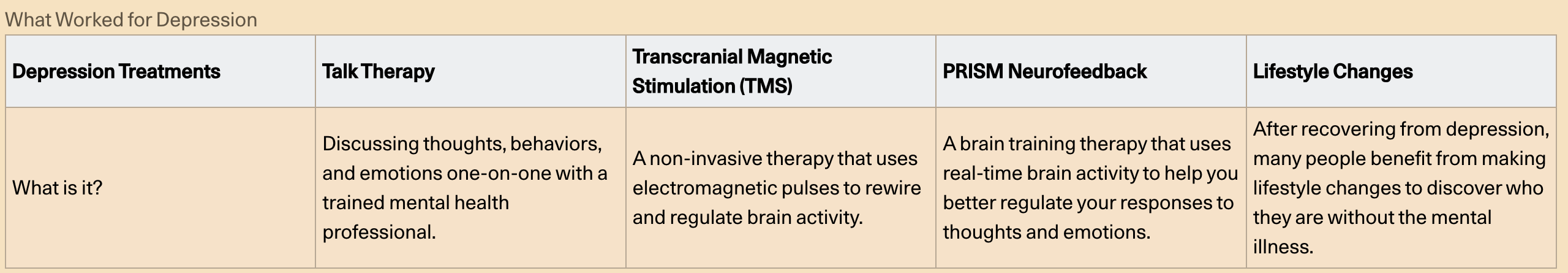
Talk therapy
Talk therapy is what we all probably think about first, when it comes to treating any mental health conditions. It’s a classic one-on-one therapy session in a quiet, safe space with a licensed mental health provider, discussing our thoughts, behaviors, and emotions. There are various types of talk therapies, and therapists often use a combination of different approaches to treat patients.
While talk therapy can be effective, only about one third of MDD cases go into remission with talk therapy alone, and more than half of individuals with MDD do not respond to talk therapy on its own at all.
That said, many find it useful during and after recovering from depression since talk therapy opens up space to explore who you are outside of MDD.
TMS therapy
TMS is a FDA-cleared therapy where a device with an electromagnetic coil is placed against the scalp. That device then sends electromagnetic waves to specific regions of the brain associated with depression, rewiring and regulating brain activity.
There are a few different types of TMS, with the two most common being traditional TMS, when you go in for 1-2 treatments per day over 6 weeks, and accelerated TMS, when you do 5-10 sessions a day for 1-6 days. Both are effective, well-tolerated, and don’t require anesthesia or significant recovery time after a session. However, accelerated TMS, particularly Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT TMS), is particularly promising, boasting a MDD remission rate of 60-80%.
PRISM neurofeedback
PRISM neurofeedback is a brain-training therapy where you use real-time brain activity feedback to learn how to control symptoms of depression. For this treatment, you wear a cap with electrodes that reads your brainwaves and translates them into audio and visual cues. The cap is connected to a computer that turns those cues into a game-like experience on a screen. You then control characters on the screen, learning what mental strategies work best in different contexts.
For depression specifically, PRISM supports the part of your brain that controls joy and motivation. In a study with 34 participants, over 78% experienced improvement in depressive symptoms, particularly anhedonia, an absence of pleasure or joy. It’s also FDA-cleared, minimally invasive, and doesn’t have as many side effects as other treatments.
Lifestyle changes
It’s no secret that lifestyle changes like eating healthier, exercising, and getting enough quality sleep reduce symptoms associated with depression. But the last thing you want to hear when experiencing what feels like an incurable depression is to “stress less” or “workout more.” MDD often makes even small lifestyle changes feel totally out of reach, and that’s where treatments like TMS and PRISM come in. They create lasting changes in the way we think, creating the right headspace to consider those lifestyle changes.
After TMS or PRISM, Tara, Browne, Ari, Stephaniei, and Kristen were finally able to make changes to their lifestyle, improving their lives and overall mental health. For Browne, this looked like more ease in attending physical therapy sessions for her chronic physical health condition. Kristen began training for a marathon, while Ari explored new hobbies and reconnected with old friends.
Common threads in depression recovery
Healing from depression looks different for everyone. Each person’s story, the treatments that work best, and how they experience depression is as unique as each of us. However, there are a few commonalities among the five mental health recovery stories above:
- Multiple modalities: For almost everyone we interviewed, talk therapy combined with another treatment, such as TMS or PRISM Neurofeedback, was what worked.
- Persistence and self-advocacy: Many treatments that work for therapy-resistant depression aren’t what insurance companies label as “first-line treatments.” To get insurance companies to cover life-changing modalities like TMS, individuals often have to be persistent and advocate for themselves.
- A ripple effect: In every story, overcoming depression had a ripple effect on other aspects of an individual’s life. Many people found new hobbies, built closer relationships, were better able to manage other health conditions, and/or went after goals that once felt impossible.
- Patience: While the right treatments change lives, finding them doesn’t happen overnight. Instead, those fighting depression often have to try many options. Even when someone finds the right treatment, progress can sometimes be slow, though it’s motivating and easier to see that progress when we document the wins along the way.
- Working with the right providers: Living with depression can be overwhelming, isolating, and at times demoralizing, especially when treatments aren’t working. The right provider can offer support, suggest new treatments, and help you manage depression, as well as discover who you are once depression is no longer in the driver’s seat. Browne reflects on her provider, “Radial has made me feel like I’m not alone. Dr. Muir has given me the motivation to try new things to help me try to improve my situation.”
Resources and support
Want to learn more about how to overcome depression? Take a deep dive:
- The Frontier Psychiatrist. Depression Can Be Over With A One Day Treatment 90% of The Time. December 27, 2024.
- Radial. PRISM Neurofeedback.
- Psychiatry and Psychotherapy Podcast. Episode 137: Ketamine Update with Brandon Kitay, MD. Released Jan 27, 2022.
- Our View Podcast. Mental Health Monday: A Conversation on Clinical Depression. March 1, 2021.
- Soft White Underbelly. A Talk On New Depression Treatments-Carlene MacMillan, M.D. and Owen Muir, M.D.. Jan 28, 2024.
The bottom line
Living with depression can feel exhausting, isolating, and sometimes hopeless. This is especially true if you’ve tried talk therapy or medications, with little improvement to show for it. Fortunately, there are other treatments out there, such as TMS and PRISM Neurofeedback, that have changed the lives of many, giving many people a chance to get to know themselves outside of their depression.
Key takeaways
- When conventional treatments like antidepressant medications don’t work, there are other options to treat major depressive disorder, as demonstrated in the above depression recovery stories.
- TMS and PRISM Neurofeedback are two of the best treatments for MDD, and they often work best when paired with talk therapy.
- Another key component is working with the right provider. At Radial, our providers work with you to explore what’s causing your depression, point you in the direction of the right treatment, and support you throughout your mental health journey.
Frequently asked questions (FAQs)
Is it possible to fully recover from depression?
Depending on the circumstances, yes. Recovering from depression is a highly unique journey, and once someone finds the right treatment modality, they are often able to recover. Some people do experience periods where the depression returns, often due to specific circumstances such as the changing of the seasons, a difficult period of life, or the loss of a loved one.
How many years does it take to recover from depression?
There isn’t a set number of years it takes to recover from depression. The timeline depends on what’s causing your depression, what treatments you try (and which ones work), and other factors unique to you.
How to rebuild your life after depression?
After overcoming depression, reflect on any habits you’d like to form, any loved ones you want to reconnect with, and new experiences you want to try. Recovery is a great time to build positive habits and put yourself out there. If all this sounds overwhelming, working with a therapist can help you navigate your thoughts, emotions, and new identity after overcoming depression.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




