What Is Treatment-Resistant Depression—And What Can You Do About It?

Having treatment-resistant depression does not mean that treatment for your depressive symptoms is out of reach. Instead, it means you may need more complex or different depression treatment options than the usual methods, which generally include antidepressants and therapy.
Everyone experiences bouts of sadness, low mood, or lack of motivation now and then. When these feelings occasionally occur but resolve, they’re frustrating but a regular part of the general ups and downs of life. After a day or two of feeling low, your mood levels out, returning to baseline.
However, if you experience persistent low mood or loss of pleasure, you may be diagnosed with major depressive disorder (MDD), an ongoing mental health condition.
To be clear, MDD is not some sort of personal failure at resiliency or being happy; it’s about your brain’s chemistry and other underlying factors, which are no fault of your own. Factors such as genetics, imbalances with neurotransmitters, hormonal dysregulation, and your life’s history (including if you’ve experienced trauma) all play a role.
About 5% to 17% of people experience MDD, which has various treatments. “Approximately 21 million people in the United States experience major depressive disorder each year,” says Colleen Hanlon, PhD, vice president of medical affairs at BrainsWay. “For comparison, that is more than the number of people living with cancer, Alzheimer’s disease, and epilepsy combined.”
Treatment-resistant depression is more common than you might think: about 30% of people with MDD have a subtype called treatment-resistant depression (TRD), which is also called treatment-refractory depression. Joshua Bess, MD, the medical director of Seattle NTC defines TRD as “a major depressive episode that has not responded to the usual treatments.” What counts as “usual treatments,” he says, is up for debate, but generally this means medication and psychotherapy haven’t helped.
Having TRD doesn’t mean you’re out of luck with finding options for easing your symptoms, though. In this article, we explore what having therapy-resistant depression, medication-resistant depression, or drug-resistant depression means. And we dig into depression treatment options, including Spravato and depression treatment without medication.
What is treatment-resistant depression (TRD)?
Treatment-resistant depression is a severe form of major depressive disorder, and it requires a more complex treatment approach than the general first-line options such as medications and psychotherapy, which are typically combined.
Dr. Bess makes an important distinction about the term. “Some have suggested calling it ‘difficult to treat depression (DTD)’ given the possibility that saying something is ‘resistant’ could mean someone is ‘resistant.’”
In other words, the “resistant” part of the current terminology does not mean that you are resistant to treatment, but that your depression hasn’t eased in response to typical go-to treatments.
“Various rubrics and scales have been developed to assess how resistant someone’s depression is,” Dr. Bess adds, “but the field seems to be settling around failure of two medications.”
Why two medications? Dr. Bess says this distinction is based on research showing that the first medication people try helps alleviate depressive symptoms about one-third of the time, and a second medication trial works even less often than that. Altogether people with depression experience improvement with two medication trials in about 60% of cases. “The remaining 40% would be TRD,” he explains.
What about psychotherapy for depression (aka talk therapy)? “While we know that medication plus psychotherapy is better than either alone,” Dr. Bess says, “a trial of psychotherapy is less clearly defined than a trial of medication, and the numbers are harder to convey clearly. So most of us use the medication trials as a shorthand.”
Why antidepressants don’t always work
“Depression is a brain disease, and the brain is an incredibly, and beautifully, complex organ,” Dr. Hanlon says. “You can think of the brain as a symphony, wherein different instruments represent different neural circuits in the brain. When everything is working well, the music sounds great. But as you can imagine, there are many things that can go wrong which make the music unpleasant.”
Research into understanding what causes depression is still ongoing. An older theory, the serotonin hypothesis, presented the concept that depression results from a deficit of serotonin, a neurotransmitter that affects mood. But newer research shows that the causes of depression are much more complex.
Analyses on the connections between serotonin levels or serotonin activity and depression are inconclusive and do not support this hypothesis. However, the hypothesis originally served as the rationale for the development of most oral antidepressants. Eventually, experiments completely disproved the role of the serotonin target in carefully designed animal models, but a whole class of oral medicines had already found their way into use.
“Medications [for depression] typically focus on increasing activity in serotonin-rich areas of the brain,” Dr. Hanlon says. “While that helps most people, many other people have a different problem going on.”
Dr. Bess offers some insights as well. “Brains are complicated,” he says. “The specific functions in the specific parts of the brain that an antidepressant acts on might improve one person’s depression, but their neighbor’s depression might be caused by some other function in some other brain area.”
He also says dosing presents challenges. “Much of the science points toward ‘if it doesn’t work at a lower dose, it probably won’t work at a higher dose,’ but there are a lot of exceptions,” he explains. “Side effects can limit doses. Drug-drug interactions can alter doses.”
Dr. Hanlon adds, “Essentially, it’s not always about how many medications someone has tried. Sometimes we need to shift the treatment method entirely and look at how we can more directly target the brain circuits involved in depression. This is where technologies like deep transcranial magnetic stimulation (TMS) come in.”
Depression can also be misdiagnosed, leading to delays in adequate treatment for what’s actually going on. “Some people who are diagnosed with depression do not have depression,” Dr. Bess says, “or they have depression that is caused by a medical problem besides ‘only’ depression.” In cases of the latter, the underlying medical problem requires treatment.
"Medical mimics" are underlying conditions that can masquerade as a psychiatric disorder. Common medical issues like thyroid dysfunction, metabolic issues, cardiac conditions, autoimmune conditions, vitamin deficiencies, side effects from medicines, and more might mimic the symptoms of various mental illnesses, easily leading to misdiagnosis.
But the bottom line is that if antidepressant medicines haven't helped you, it’s not your fault; it’s simply that your depression may require a more nuanced approach.
What are the symptoms of treatment-resistant depression?
Treatment-resistant depression symptoms are the same as those for major depressive disorder order. However, with TRD, symptoms may be more severe. They can include:
- Anhedonia (reduced ability to experience pleasure)
- Anxiety
- Appetite changes
- Depressed mood
- Fatigue
- Feelings of worthlessness
- Irritability
- Lack of motivation to engage various activities
- Lengthy depressive episodes
- Restlessness
- Sleep disturbances (e.g., insomnia or excessive sleeping)
- Suicidal thoughts or behaviors
What causes treatment-resistant depression?
Researchers haven’t found a definitive cause of treatment-resistant depression. Instead, several factors likely contribute. Here are a few considerations.
Brain chemistry and circuitry
Like houses on a street, no two brains are exactly the same. Sure, they have similar features, but several factors can cause variations in brain functioning. Here are a few examples.
- Hypothalamic-pituitary-adrenal (HPA) axis dysfunction: This neuroendocrine system controls your stress response, and when it becomes dysregulated (for example, as a result of trauma), its overactivation can contribute to depression and make it harder to treat.
- Neurotransmitter dysfunction: Although alterations in neurotransmitters may contribute to depression in some people, they may not be the cause, leading to depression that goes untreated with standard medications.
- Limited neuroplasticity: Your brain is constantly adapting and forming new neural connections. These adaptations and changes are referred to as neuroplasticity, which may be impaired in some people. Brains need to be able to change to benefit from treatments that can cause a change, with new research focusing on this problem recently.
- Inflammation: More research is needed on this topic, but newer research suggests the immune system, specifically inflammation, may play a role in some cases of depression, making it harder to treat with standard medications. Inflammation can even play a role in the response to treatments like TMS, other new research found. Psychedelic medicines like psilocybin might even provide some of their effects via their anti-inflammatory properties.
Psychological stressors
Our life experiences and the environments we live in can contribute to the development of depression and make treatment more complicated.
- Adverse childhood experiences (ACEs): ACEs involve any traumatic experience in childhood, such as abuse, neglect, having an incarcerated parent, or experiencing poverty, systemic racism, a natural or manmade disaster, school shooting, etc. ACEs cause alterations in how we respond to stress. ACEs are linked to more severe symptoms of depression.
- Chronic stress: Our stress response exists to keep us safe in the face of a true threat, like having to fight off an attacker. But when you experience chronic (ongoing) stress, it can have a negative effect on the HPA axis and potentially lead to inflammation, which may impact how well you respond to antidepressants.
Genetics and epigenetics
You may be genetically predisposed to developing TRD, or environmental stressors may change how your genes are expressed (how they work), potentially leading to TRD.
- Genetic predisposition: One study looked at genetic data from nearly 300,000 participants. The researchers found an association between TRD and polygenic scores, a number that estimates one’s genetic predisposition for a trait or condition. People with the genetic predisposition for neuroticism, insomnia, and negative emotional impairment were more likely to develop TRD.
- Epigenetics: We inherit our genes from our biological parents. However, our environment and other factors can change how those genes work. Epigenetics is the turning “on” or “off” of genes based on these factors, and recent research suggests that epigenetics plays a role in the development of MDD—and potentially TRD. Lifestyle interventions can have a dramatic effect on epigenetics and help explain why these interventions can be powerful treatments for depression.
Other mental health conditions
You may have other mental health conditions that make your depression symptoms more severe or hard to treat. These include anxiety, personality disorders, post-traumatic stress disorder (PTSD), and more.
What are the risk factors for treatment-resistant depression?
The risk factors for TRD fall under several categories. “Even people with several risk factors will be put through the ‘usual’ treatments first,” Dr. Bess says. “So these serve as a possible explanation of why something did not work and/or a caution when we are advising patients about the likelihood that the next treatment trial will help.”
Clinical risk factors for treatment-resistant depression
- Early age of depression onset
- Longer episode duration
- More severe symptoms
- Psychotic features
- Other psychiatric disorders (e.g., anxiety, personality, substance use)
- History of poor antidepressant response
- Non-adherence to medications
Biological and medical risk factors for treatment-resistant depression
- Family history of mood disorders or treatment resistance
- Chronic illness (e.g., diabetes, cardiovascular disease, or pain and neurological conditions)
- Inflammation and immune system dysregulation
- Brain changes
- Alterations in how you metabolize certain medications
Psychosocial risk factors for treatment-resistant depression
- Childhood trauma
- Ongoing psychosocial stressors (e.g., financial, job, relationship issues)
- Limited social support
Treatment related risk factors for treatment-resistant depression
- Inadequate dose or duration of antidepressant trial
- Treatment not optimized with a combination of strategies
- Limited access to psychotherapy or interventional treatments
.png)
How is treatment-resistant depression diagnosed?
“The only way to diagnose TRD,” Dr. Bess says, “is a good old-fashioned interview. It is important to get as detailed a history as possible, which can be very challenging because it is difficult for people to remember lots of details, especially when they have had serious mood episodes in the past.”
Your clinician may ask you when you first noticed your symptoms, how they show up for you, what treatments you’ve tried and whether they helped somewhat or not at all. They may also ask you about any other medical conditions, your family medical history, your life experiences, your living situation, and more. It’s also considered good practice to give you questionnaires that help assess the severity of your symptoms.
“People also tend to have their own ‘narrative’ about their depression or other psychiatric history—not a fictional narrative, but their own way of having put all the pieces together over the years,” Dr. Bess says. “I do my best to start from the beginning and not make any assumptions.”
He adds that the patient’s point of view is an important part of the diagnosis process. “I am not saying they get to diagnose themselves,” he explains, “but for a diagnosis to be helpful/useful, the patient must have at least some buy-in.”
Diagnosis can be tricky for several reasons. “There is often stigma, self-blame, and/or change in perception about one’s future options,” Dr. Bess says. “And, besides having a code to put into a blank on an insurance form, it is only useful if it then informs what the next steps in assessment and treatment might be.”
How is treatment-resistant depression treated?
The condition name—treatment-resistant depression—doesn’t inspire confidence in finding symptom relief. But, as Dr. Hanlon puts it, “’Treatment-resistant’ doesn’t mean untreatable.” It just means treatment requires a different approach than standard medications and psychotherapy.
Dr. Bess agrees, acknowledging that people with TRD have often tried many treatments only to become frustrated or left hanging. “Sometimes they have been told ‘I don’t have anything else to offer you’ by their psychiatrist or another professional,” he says.
“In reality, by the time someone is in my office, they are ‘done’ with more medication or more therapy,” he adds, “but it is important to keep in mind that sometimes a person just has not had adequate treatment trials under the supervision of a real expert.”
The following is a list of potential treatments for TRD. It includes medications that are approved or cleared by the Food and Drug Administration (FDA), and those that providers sometimes prescribe off-label for the condition, which means the treatment isn’t explicitly approved for TRD but may have some benefit.
Questions to ask your provider about treatment options
- What are the potential risks and side effects?
- When will I see results?
- How long do I use this treatment?
- Will my insurance cover this?
- What will my out-of-pocket costs be?
- Who is a good candidate for this type of treatment?
- Who is not a good candidate for this type of treatment?
- What are the results in clinical trials?
- What are the long-term considerations of trying this treatment?
- Do I take this treatment at home, or do I come in for an appointment?
- How is the treatment administered?
Medications
SSRI, SNRI and atypical anti-depressants (Remeron/mirtazapine, Wellbutrin/bupriopion, AUVELITY, etc) may be considered if not previously trialed at a therapeutic dose or duration. Providers will often trial medications like Wellbutrin or Remeron as “add-on” treatments to boost the effect of an SSRI/SNRI before moving to other drug categories.
Atypical antipsychotics: Including aripiprazole (Abilify), brexpiprazole (Rexulti), quetiapine (Seroquel) and olanzapine (Zyprexa)
- What it is: These medications are atypical antipsychotics.
- How it works: While many antidepressants target just one or two neurotransmitters, adding an antipsychotic to a treatment regimen helps target more receptors or neurotransmitters and can be especially beneficial for helping to treat TRD when another mental health condition is present.
- What it’s FDA-approved to treat: All these medications are approved as an “add-on” treatment for MDD, with olanzapine specifically approved in combination with fluoxetine (Prozac) for TRD. Aripiprazole and risperidone are also approved for treating schizophrenia, bipolar disorder, and autism-related irritability. Brexpiprazole is also approved for treating Alzheimer’s disease-related agitation. Quetiapine and olanzapine are also approved for treating schizophrenia and bipolar disorder.
Esketamine nasal spray (Spravato)
- What it is: This new depression medication is a form of ketamine, administered as a nasal spray.
- How it works: Spravato treatment blocks NMDA receptors in the brain, which are part of the glutamate neurotransmitter system. This helps increase brain neuroplasticity, which helps repair and improve neural pathways. Esketamine helps reduce the risk of depressive symptoms returning. “This is where all the sexy things are happening in psychiatry,” says Dr. Bess. “Ketamine, and its cousin esketamine/Spravato® nasal spray, is offering relief to people in record time. It doesn’t ‘last’ unfortunately, so we need to work out reliable maintenance protocols or adjunctive medications to help with durability.”
- What it’s FDA-approved to treat: Esketamine is approved for the treatment of treatment-resistant depression (TRD) in adults. It can be used alone or in conjunction with an oral antidepressant. It’s also approved for treating MDD (in combination with an antidepressant) when a patient has suicidal ideation or behavior.
- What it is: Lithium is a mood stabilizer.
- How it works: Lithium influences neurotransmitter levels in the brain, including serotonin, dopamine, and gamma-aminobutyric acid (GABA).
- What it’s FDA-approved to treat: Lithium is approved to treat bipolar I disorder and can help reduce symptoms during manic or mixed episodes. However, some providers prescribe lithium off-label as an add-on therapy for MDD and schizophrenia.
MAOIs (monoamine oxidase inhibitors)
- What it is: MAOIs are some of the earliest antidepressants developed. They include Isocarboxazid (Marplan), Phenelzine (Nardil), Selegiline transdermal system (Emsam), and Tranylcypromine (Parnate).
- How it works: MAOIs work by blocking the action of monoamine oxidase, which is an enzyme that breaks down certain neurotransmitters related to mood. By inhibiting this enzyme, these medications increase neurotransmitter levels. MAOIs should never be taken with other SSRI/SNRIs and generally require dietary restrictions.
- What it’s FDA-approved to treat: Isocarboxazid is approved to treat MDD. Phenelzine is approved to treat various types of depression including TRD. Selegiline is a transdermal patch that is approved for MDD treatment. Tranylcypromine is approved for MDD, but it tends to be used as a “last-resort” medication because of its potential for serious side effects and food and medication interactions.
- What it is: Pramipexole is a dopamine agonist.
- How it works: It works by activating dopamine receptors, helping to improve signaling of this neurotransmitter. It has shown promise for TRD by boosting mood and increasing motivation.
- What it’s FDA-approved to treat: Pramipexole is approved for treating Parkinson’s disease and restless leg syndrome. However, providers sometimes prescribe the medication off-label for TRD.
Psilocybin
- What it is: Psilocybin is a compound found in certain psychedelic mushrooms. It converts to psilocin in the body, causing hallucinogenic effects when taken at specific doses.
- How it works: Psilocin activates certain serotonin receptors, which produces temporary alterations in brain network connectivity and communication and increases neuroplasticity. The various mechanisms may help with processing trauma, easing depressive symptoms, and more. “In some parts of the country, laws pertaining to possession and use of psychedelic drugs have been relaxed or ‘decriminalized’ and there has been significant growth in available training programs for psychedelic psychotherapists,” Dr. Bess says. “In most cases, the model is a patient who takes the psychedelic as part of psychedelic-assisted-psychotherapy.”
- What it’s FDA-approved to treat: Psilocybin is not FDA-approved. However, the government agency has granted Breakthrough Therapy designation to certain pharmaceutical companies to fast-track research and development. Ultimately, therapeutic use of psilocybin for TRD is still undergoing extensive research, though the results show promise. At present, it can be used legally in two states—Colorado and Oregon.
Psychotherapy
If you have TRD, you may have tried psychotherapy already. But here are a few techniques that have efficacy for helping with the condition. The FDA does not approve or clear therapy modalities.
- Cognitive behavioral therapy (CBT): CBT helps you recognize and reframe negative thought patterns.
- Dialectical behavioral therapy (DBT): DBT is like CBT in that it helps you recognize and change unhelpful patterns or behaviors, but it also helps you with emotional regulation, mindfulness, and acceptance of emotions and situations.
- Mentalization-based treatment (MBT): MBT helps you become more aware of how your various mental states influence your thoughts, emotions, and behaviors. This can help you also better understand dynamics in your interpersonal relationships.
- Interpersonal psychotherapy: This type of talk therapy focuses on relationship improvement to help you reduce related psychological distress.
- Family or couples therapy: This type of therapy includes your family members or your romantic partner in the process to help improve relationship dynamics.
- Group psychotherapy: With group therapy, you’ll undergo therapy with others who have similar symptoms or have experienced similar situations in their lives.
- Behavioral activation: This form of therapy focuses on increasing your engagement in healthy activities or behaviors, including those you find rewarding or pleasurable, so as to boost mood.
Interventional treatments for depression
Transcranial magnetic stimulation (TMS):
- What it is: TMS is a safe, effective procedure that uses magnetic fields to stimulate nerve cells in specific areas of the brain in order to “rewire” neurological patterns.
- How it works: The electrical stimulation alters neuronal activity, which can help improve depressive symptoms. “When we apply TMS to the neural circuits that are ‘too quiet’ or ‘playing out of sync,’ these patients are often able to find remission from their depression for the first time,” Dr. Hanlon says.
- FDA notes: Devices used for TMS typically undergo clearance rather than approval. The FDA first cleared a TMS technology for MDD in 2008, specifically for adults who have not responded to antidepressants. As of today, TMS is FDA-cleared for major depressive disorder in both adults and adolescents, anxious depression, OCD, migraines, and smoking cessation.
Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT TMS)
- What it is: SAINT is a nonsurgical outpatient procedure that delivers magnetic pulses to areas of the brain that are linked to depression.
- How it works: The pulses address abnormal brain signals, and your clinician customizes the treatment to your specific needs based on brain imaging.
- FDA notes: In 2022, the FDA cleared the SAINT system created by Magnus Medical.
Electroconvulsive therapy (ECT)
- What it is: ECT is the delivery of a dosed electrical current to induce a controlled seizure while under general anesthesia. This procedure uses a pulse of electricity to cause neural circuits to activate. ECT typically is administered three times a week (M, W, F) over 2-4 weeks.
- How it works: The procedure produces changes in brain chemistry, which may improve depressive symptoms.
- FDA notes: Devices used for ECT typically now undergo clearance rather than approval. Various devices have been cleared.
- ECT became popularized in the 1940s when technology for dosing the electrical current and access to rapid acting general anesthesia medications were not yet available. At that time, ECT had significant side effects and stigma. Big changes were made to the procedure in the 1980s leading to a re-emergence of ECT treatment. Under newer treatment protocols, ECT has become a humane, effective and widely-accepted treatment for severe mental illness, including TRD
Deep brain stimulation (DBS)
- What it is: This surgical treatment involves the implantation of a small device (with electrodes going in the brain, a battery in the chest, and a wire connecting them).
- How it works: The setup sends continuous electrical pulses to targeted brain areas to help address symptoms.
- FDA notes: DBS devices receive either FDA approval or clearance. Devices have been approved or cleared for epilepsy, Parkinson’s disease, essential tremor, and dystonia. As of now, no devices have been approved or cleared for TRD. However, clinical trials are underway.
Prism MDD
- What it is: This noninvasive neurofeedback device uses electroencephalogram (EEG) and machine learning.
- How it works: Prism MDD tracks your brain activity with EEG while you’re interacting with a computer simulation. The simulation provides you feedback for regulating your thought patterns, especially those related to your reward system pathways, to help address anhedonia.
- FDA notes: The FDA granted clearance to the GrayMatters Health Prism MDD device for treating PTSD. Clinical trials are in the works for treating MDD, but some clinicians administer the procedure off-label.
External Combined Occipital and Trigeminal Afferent (eCOT-AS)
- What it is: This is a noninvasive wearable technology for at-home use.
- How it works: The Proliv™Rx device is a headset that delivers electrical pulses to specific nerve pathways in your head, including to the occipital and trigeminal nerves.
- FDA notes: Proliv™Rx is currently undergoing regulatory review with the FDA.
Rejoyn
- What it is: Rejoyn is an app featuring brain-training exercises to activate specific parts of the brain that may not be activating properly in some people with depression.
- How it works: The app's brain-training exercises activate the feeling part of the brain (the amygdala) and the thinking part of the brain (prefrontal cortex) to help them work better together.
- FDA notes: The FDA cleared the Rejoyn app in 2024.
The bottom line
A diagnosis of treatment-resistant depression can be frustrating, but it does not mean that treatment isn’t possible, only that you may require different modalities than the standard first-line options to help alleviate your symptoms.
TRD is common; affecting about 30% of people suffering from depression who are prescribed medications and receive psychotherapy. A knowledgeable provider can evaluate your situation and help you find the right treatment plan so you can get back to feeling more like yourself.
Key takeaways
- Treatment-resistant depression is a subtype of major depressive disorder.
- Having treatment-resistant depression means that your depressive symptoms have not improved despite first-line treatments such as antidepressants or psychotherapy.
- However, having treatment-resistant depression does not mean that your symptoms can’t be treated—only that you may need a more novel approach than the usual methods.
- If you have tried 2 or more medications without significant improvement, it is unlikely that trying additional medications will have a different result. Trying more targeted treatments, like TMS, is more likely to lead to symptoms remission and functional improvement.
- Radial can help. Sign up online and undergo a consultation to see what’s possible.
Frequently asked questions (FAQ’s)
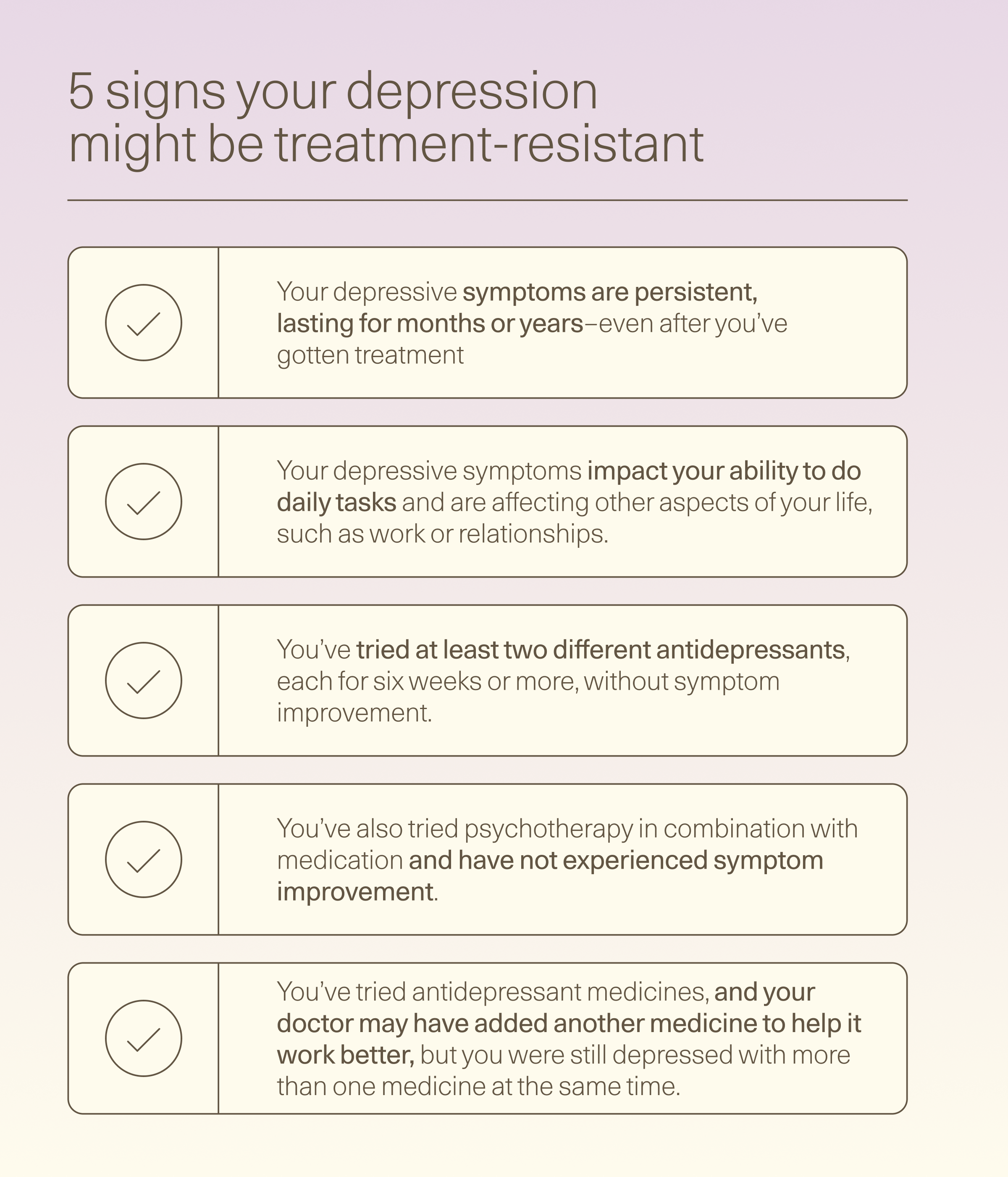
What are signs of treatment-resistant depression?
You might have treatment-resistant depression if your depressive symptoms are persistent, impact your ability to do daily tasks, and are affecting other aspects of your life; you’ve tried at least two different antidepressants; and you’ve also tried psychotherapy in combination with medication and have not experienced symptom improvement.
What can be done for treatment-resistant depression?
Although the name implies that treatment-resistant depression is resistant to treatment, what it really means is that you haven’t experienced symptom improvement from the traditional treatments of antidepressants and psychotherapy. Other new treatments are available, including TMS, different types of medications, and some medical procedures.
Can treatment-resistant depression be prevented?
Although researchers haven’t pinpointed the exact causes of treatment-resistant depression, several factors likely play a role, including genetics or how your genes work, your life experiences, your brain chemistry, and more. We don’t have control over these factors, so major depressive disorder (MDD), which is a mental health condition, cannot be prevented. Treatment-resistant depression is a subtype of MDD.
Why does depression make you tired?
Depression can make you feel tired or as if you have minimal energy because of disrupted neurotransmitter function, which can impact mood, lower motivation to engage in activities, and disrupt sleep.
Deep dive recommendations:
- Huberman Lab Podcast. Dr Paul Conti: Therapy, Treating Trauma & Other Life Challenges. Release June 6, 2022. https://www.hubermanlab.com/topics/mental-health#mental-health---mental-health-therapies-and-treatments
- Huberman Lab Podcast. Dr. Nolan Williams: Psychedelics & Neurostimulation for Brain Rewiring. Released: Oct 10, 2022. https://www.hubermanlab.com/episode/dr-nolan-williams-psychedelics-and-neurostimulation-for-brain-rewiring?timestamp=556
- Metabolic Mind Podcast. The Truth About Treatment-Resistant Depression: Part Two (TMS and Psychedelics). Released August 20, 2025. https://podcasts.apple.com/podcast/id1678826858?i=1000722845329
- Psychiatry and Psychotherapy Podcast. Episode 155: Is Depression a Chemical Imbalance? https://www.psychiatrypodcast.com/psychiatry-psychotherapy-podcast/episode-155-is-depression-a-chemical-imbalance
- Psychiatry and Psychotherapy Podcast. Episode 235: The Serotonin Hypothesis: Controversies and Nuance with Awais Aftab, MD. https://www.psychiatrypodcast.com/psychiatry-psychotherapy-podcast/episode-235-serotonin-hypothesis-controversies-awais-aftab
- Psychopharmacology and Psychiatry Updates Podcast. TMS for Depression: From Clinical Trials to Results. Released April 16, 2025. https://psychopharmacology.libsyn.com/tms-for-depression-from-clinical-trials-to-results
- The Frontier Psychiatrist Podcast. Accelerated Transcranial Magnetic Stimulation (aTMS), Explained. Released May 13, 2024. https://podcasts.apple.com/us/podcast/the-frontier-psychiatrists/id1577248149?i=1000655423684
- Soft White Underbelly. Insurance-Covered Treatments For Depression, Anxiety, OCD and PTSD-Owen Muir, M.D. https://youtu.be/tUk2860mlYY
- Soft White Underbelly. A Talk On New Depression Treatments-Carlene MacMillan, M.D. and Owen Muir, M.D.https://youtu.be/1PRZbJeQ5AU
- Tim Ferriss. My 2 Sessions of Transcranial Magnetic Stimulation for OCD and Anxiety. https://www.youtube.com/watch?v=iSZnzNLhxCc
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




