What Is TMS Therapy? Benefits, Side Effects, and Results
.png)
Transcranial magnetic stimulation (TMS) therapy uses magnetic pulses to help rewire and regulate brain activity. It has many of the qualities you’d want in a mental health treatment: it’s backed by years of research, offers quick response time, has minimal side effects, and is FDA-cleared.
Let’s unpack why TMS works for depression, OCD, and other conditions—even when medications and other treatment options don’t.
Transcranial magnetic stimulation (TMS) therapy is a noninvasive treatment, most commonly used for depression, where an electromagnetic coil is placed near the scalp. The coil uses magnetic pulses to adjust activity in specific regions of the brain. It works differently from more traditional psychiatric treatments, such as talk therapy and medications, and the treatment’s uniqueness can feel intimidating at first. But it’s also the reason TMS helps so many.
Take "Harriet", for example — we've changed her name to protect her privacy. She’s a 20-something professional who has struggled with depression, has been in talk therapy, and has been taking a variety of medications. After multiple failed treatments, a mental health provider recommended TMS.
“After two weeks of TMS, it was like the weight of the depression significantly started to lift for her,” says MaryEllen Eller, MD, regional medical director at Radial and a psychiatrist involved in Harriet’s treatment, “She started reporting having more energy and being able to take better care of herself, which was a dramatic improvement over the past few months.” After three weeks, Harriet told her therapist she no longer had suicidal thoughts.
Harriet’s story isn’t an outlier. With newer TMS protocols like SAINT, up to 60-80% of people experience remission of their depression after four weeks, and this treatment works for OCD, depression, smoking cessation, and many other conditions.
What is TMS therapy?
TMS is a safe and effective way to treat conditions like depression and OCD that uses precise and targeted electromagnetic stimulation to create lasting changes in different regions of the brain.
Admittedly, the idea that a magnet could influence our brains is difficult to grasp, and the medical community is still researching the exact mechanics of TMS. But we do have a solid understanding of the basics (plus decades of clinical studies proving a high TMS success rate, but more on that later).
To understand how a TMS works, we have to bring it back to physics 101, specifically magnets and electricity. Any object that generates its own magnetic field qualifies as a magnet, whether it’s that fridge magnet bought on last summer’s vacation to the much stronger electromagnetic coil in a TMS device. During TMS, electricity is used to turn the coil into a powerful and precise magnet, hence the name electromagnetic coil.
Neurons communicate with one another throughout the body via tiny electrical impulses. When the TMS device is close to the scalp, targeting the areas associated with the condition being treated, the electromagnetic coil influences the brain’s electrical activity. It delivers rapid, repeated pulses of a strong electromagnetic current, stimulating the brain.
“TMS strengthens the connections between the emotion center and the thinking and planning center, and those are the connections that break down under stress and depression,” says Chris Aiken, MD, a psychiatrist and medical editor of the Carlat Psychiatry Report, “It's a bit like weight lifting for the brain. If you lift weights every day your muscles grow. Not right away, but gradually. With daily TMS, the neural connections grow and strengthen.”
.png)
How does TMS work?
The idea of a non-invasive, effective treatment that creates lasting changes sounds great in theory, but how does it actually work?
TMS is delivered through a TMS machine, an electromagnetic device, usually in the shape of a cap, that rests close to your scalp. The cap houses a coil that delivers brief, focused magnetic pulses that pass through the skull and induce tiny electrical currents in specific regions of the cortex. Repeated in carefully timed trains over multiple sessions, these currents fine-tune the activity of mood-related circuits, producing durable changes in the neural pathways.
“For TMS, you're sitting comfortably in a chair with a funny little hat on your head,” says Dr. Eller, “You may hear a woodpecker type noise, feel some tingling on your scalp, but it's rarely painful, it's not invasive, and it's not super loud.”
Each TMS session is quite short, lasting less than ten minutes, though you may undergo multiple sessions per day. TMS has been FDA-cleared since 2008 and is safe and effective, with minimal side effects or discomfort during sessions.
Types of TMS therapy
When we think of antidepressants, specific medications come to mind, like fluoxetine (Prozac) and sertraline (Zoloft). TMS works the same way; it isn’t one specific therapy but a group of treatments.
Under the TMS umbrella, there’s:
- Repetitive TMS (rTMS): Typical TMS protocol that delivers repeated electromagnetic pulses to targeted areas of the brain.
- Theta Burst Stimulation (TBS): A patterned version of TMS that's meant to mimic natural brain rhythms. Because each train is shorter, a full session usually lasts three to ten minutes instead of the twenty or more required for standard rTMS.
- Deep TMS (dTMS): Uses a differently shaped coil (for example, the BrainsWay H-coil) that penetrates deeper brain regions.
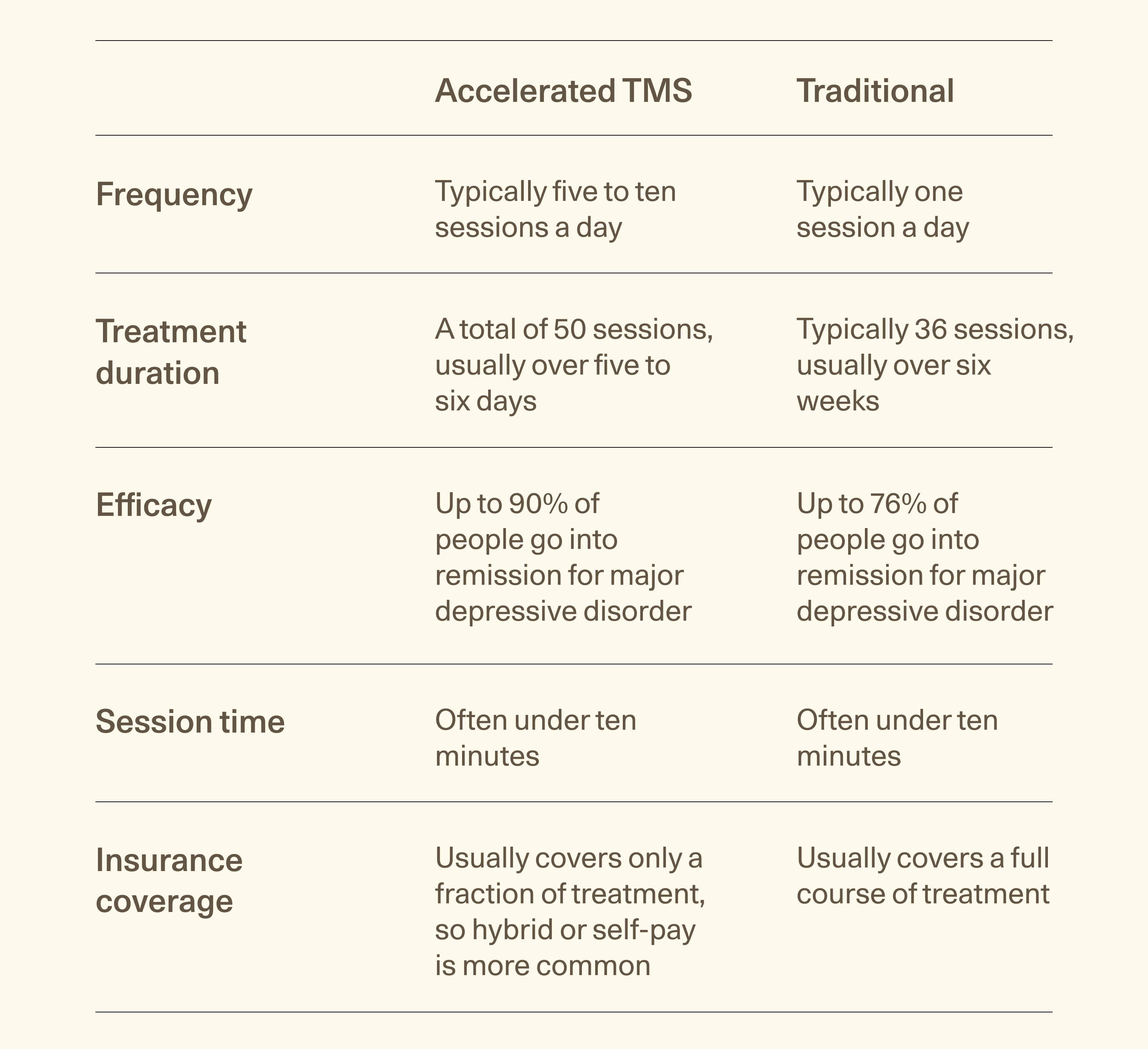
- Accelerated TMS: Any of the above protocols delivered multiple times per day on a condensed schedule, often five to ten sessions daily for about a week, to speed clinical response.
Accelerated vs traditional
Since scientists started researching TMS in the late 20th century, it’s always been an effective, safe treatment. But the development of accelerated TMS, particularly the introduction of Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT TMS), stimulated a breakthrough (pun intended).
“SAINT TMS more than doubles the recovery rates, bringing up to 90% of people to remission, and these are people who did not respond to any other treatment,” explains Dr. Aiken, “SAINT TMS is also faster, as the treatment takes five days instead of six weeks.”
While SAINT TMS has been available for a few years, it isn’t offered by every TMS provider. Magnus Medical has a search engine to find centers offering SAINT TMS, and you’ll find Radial’s centers in the search results.
Conditions TMS can treat
Currently, TMS is FDA-cleared for obsessive compulsive disorder (OCD), different types of depression, smoking cessation, and migraines, but it’s effective for other purposes too.
FDA-cleared uses
The FDA has approved or cleared TMS devices for various conditions. FDA-approved devices undergo a rigorous process to test safety and efficacy, when it’s a brand new or risky technology, for treating a specific condition. For lower-risk devices, manufacturers can use the FDA 510(k) clearance pathway by showing their device is as substantially equivalent to one already on the market. For us non-medical folks, there isn’t a huge difference between the two.
TMS is FDA-cleared for:
- Major depressive disorder (both in adults and adolescents)
- Anxious depression
- OCD
- Migraines
- Smoking cessation
Emerging uses
TMS is safe and effective for other conditions that the FDA has yet to approve or clear:
- PTSD
- Postpartum depression
- Bipolar disorder
- Schizophrenia (specifically for auditory hallucinations)
- Addiction
- Parkinson’s disease
- Stroke recovery
.png)
Who is a good candidate for TMS treatment?
“The best patients for TMS are patients who have severe or moderately severe depression, but are still motivated enough to go into their doctors office for treatment three to five days a week,” says Aron Tendler, MD, a psychiatrist in West Palm Beach, Florida, “If they cannot do that, they either need electroconvulsive therapy (ECT) in a hospital or medications.”
Dr. Eller adds it’s also a great option for those with OCD who haven’t found relief from therapy or medication alone. TMS is promising for many other conditions (see list of emerging uses above), but insurance typically only covers treatment for FDA-cleared uses.
Who should not get TMS treatment?
TMS isn’t the right fit for everyone. If you have any iron-containing metal implants in your brain (think:, cochlear implants, metal plates, and implanted pacemakers), the implant may disrupt TMS treatment. TMS, with FDA-cleared high frequency stimulation,isn’t safe for those with a history of seizures, since a seizure is a potential—but very rare—side effect.
TMS effectiveness
As Harriet’s story demonstrates, TMS is effective. To better understand just how amazing this therapy is, let’s look at the TMS success rate for a range of conditions.
Depression outcomes
Major depressive disorder (MDD) is the most common reason people turn to TMS therapy. And the results speak for themselves; even when medications fail, TMS can make a lasting difference:
- Over 81% of those with MDD improve within 20 sessions of deep TMS
- Another study suggests the response rate is as high as 82%
- 65% experience lasting remission after 30 sessions, meaning depression disappears entirely
OCD outcomes
For people living with OCD, TMS offers life-changing results. About 58% of OCD patients respond to TMS. Plus, OCD patients are three times as likely to experience reduced symptoms with TMS than a sham.
Migraine outcomes
TMS may reduce the severity and frequency of migraines, though researchers are still learning how well it works. TMS is also promising since it has fewer side effects and risks than other treatment options.
Smoking cessation outcomes
It’s no secret that it's difficult to quit smoking. Smoking cessation medications offer a 15.7-21.8% six month abstinence rate. TMS’ rate of smoking cessation at the end of treatment (six weeks) is 25.3% and it has fewer side effects.
Other outcomes
And what about other medical conditions? TMS shows hope for seven others, with early research studying the following conditions:
- PTSD: TMS leads to marked improvement for those with PTSD.
- Postpartum depression: After TMS, the depression scores of people with postpartum depression in ten different clinical trials improved by 59%. In one of those trials, the remission rate was also 59%.
- Schizophrenia: TMS improves executive function and decision-making in those with schizophrenia.
- Addiction: TMS may reduce the number of cue-induced cravings for those with a drug addiction.
- Parkinson’s disease: People with Parkinson’s may experience improved cognitive function and walking ability, as well as fewer depressive symptoms after TMS.
- Stroke recovery: Gait and muscle strength improved moderately for patients recovering from a stroke.
- Bipolar disorder: TMS may help reduce depressive symptoms with a lower risk of triggering mania.
TMS side effects and safety
As if there weren’t enough reasons to love TMS therapy, it also has minimal side effects, especially compared to antidepressants and other psychiatric interventions like electroconvulsive therapy. The latter can lead to memory loss and requires anesthesia. With TMS, you’re fully conscious the entire time with no shocks, pain, or forgotten memories.
Common side effects
The most common “side effect” is that people feel better. TMS changes how someone shows up and what emotions they feel—and this side effect lasts long after sessions end.
Physical side effects are typically minor and short lived. Some people experience mild headaches and scalp or neck pain. These common side effects typically go away on their own or with over-the-counter medications like Tylenol and lessen as sessions continue.
Uncommon side effects
Some report feeling fatigued or lightheaded after first starting treatment. The treatment also occasionally causes mild anxiety and temporary insomnia. A drop in blood sugar can occur, so if you take insulin, it’s worth checking levels after.
The most serious potential side effect is seizures. This risk is extremely low—fewer than 1 out of 1,000 patients experience it, which is less than 0.1%.
What to expect before, during, and after TMS
Not knowing what to expect can make any medical treatment overwhelming, and TMS is not an exception. To avoid any pre-TMS dread, here’s what to expect prior to, during, and after your treatment.
Pre-treatment screening
Before starting, you’ll meet with a mental health provider trained in TMS, typically a psychiatrist, mental health nurse practitioner, or physician assistant. They will assess symptoms, medical history, and previous treatments to determine if TMS is a good fit.
Aside from attending that initial screening, there’s nothing else you need to do to prepare. You can eat normally, drive to and from your sessions, and won't be put to sleep during TMS.
Session experience
TMS is performed in a TMS therapy center with licensed technicians operating the device and overseeing treatment. The treatment space is designed to be calming, and there’s nothing you have to do during treatment. “You could be listening to music, relaxing, or just chatting with the technician during treatment,” says Dr. Eller.
Many people say the sensation is weird, but not painful. “It's a unique feeling that might take you a moment or two to get used to, but isn't going to cause significant pain,” Dr. Eller explains, “It doesn't leave any marks or redness either.”
Depending on the recommended treatment course, patients undergo 30-50 sessions of TMS. Many describe a moment where the depression just disappears during treatment, almost like an off switch.
Researchers call this the “first response rate,” and one study placed it at about 18.5 sessions for OCD. That doesn’t mean you stop once you experience that first response. The benefits keep coming throughout the recommended number of sessions.
Post-treatment
Once the switch has been turned off, so to speak, you have an opportunity to establish a new lifestyle. “TMS helps your brain lay down new brain connections, which helps those healthy lifestyle habits stick better in your brain,” explains Dr. Eller.
Post-TMS is the time to implement healthy routines which were hard to follow before, such as getting morning sunlight or meditating in the evening. Dr. Eller also adds that many people find talk therapy useful after TMS to reinforce changes.
How TMS compares to other treatments
“TMS is better tolerated, it has less side effects, the benefits last longer, and we can see the benefits more quickly than if we were to just do medications or psychotherapy,” says Dr. Eller. Here’s more on how TMS compares to (and can work in tandem with) standard antidepressants, talk therapy, and ECT.
TMS vs. medication
“If your antidepressant isn't working, TMS offers a much better chance of recovery than changing antidepressants or adding new medications like an antipsychotic (eg, aripiprazole),” says Dr. Aiken. He adds that TMS is also better tolerated than most medications and has fewer side effects.
It may also be safe to take medications alongside TMS, though some medications, such as benzodiazepine and antipsychotics, are likely to disrupt the response to TMS. A psychiatrist or psychiatric NP should evaluate the safety of combining medication and TMS before starting treatment.
TMS vs. talk therapy
Transcranial magnetic stimulation and talk therapy are teammates rather than rivals. The brief magnetic pulses of TMS prepare brain circuits for change, while psychotherapy or cognitive behavioral therapy supply the strategies and insights that turn that readiness into lasting progress. Used together, they often deliver more durable relief than either treatment can achieve on its own.
“TMS is a way of optimizing the improvements that you can get in psychotherapy,” explains Dr. Eller, “It helps all of those positive changes stick in the brain by giving your brain the ability to lay down new connections more quickly and to hold those connections over a long period of time.”
TMS vs ECT
TMS is often mistaken for electroconvulsive therapy (ECT) because both are forms of brain stimulation, yet the two procedures are fundamentally different . On the surface, the two sound similar but there are some key differences.
ECT delivers an electrical current while the patient is under general anesthesia, intentionally producing a brief seizure that can alleviate severe depression and other conditions. By contrast, TMS applies focused magnetic pulses through a coil placed on the scalp, requires no anesthesia, and does not trigger a seizure.
In rare cases, ECT can also cause side effects like memory loss, confusion, nausea, and muscle soreness, which are more severe than TMS’ most common side effects.
TMS logistics: Cost, insurance, and accessibility
The cost of TMS therapy could be a potential barrier for some, but it’s important to note that insurance may cover a large portion of your TMS treatment. Government-sponsored insurance often covers TMS when certain criteria are met. Medicare, for example, covers TMS for those with major depressive disorder or OCD who have failed at least one medication.
As is usually the case with private insurance, determining if a private policy will cover TMS is complicated. That said, Dr. Eller outlines when insurance companies are most likely to cover TMS:
- There’s a diagnosis of a condition that has an FDA-cleared indication.
- That condition has been resistant to at least two different medications or someone couldn’t take medication because of the side effects
- Evidence of psychotherapy, either completed or ongoing, without remission
- No history of seizures or certain neurological conditions
- A clinician trained in TMS conducted an assessment, recommending TMS, with a Board-certified psychiatrist as a supervisor.
More insurance plans cover the entire TMS therapy cost for traditional TMS, but usually only cover part of the price for accelerated treatment. Some insurers now cover accelerated treatment if medically necessary, but prior authorization is usually required.
In general, at a Radial treatment center, patients most commonly pay a $10-$50 copay each day of treatment, or pay 10%-30% coinsurance. Self-pay treatment cost for a full course of TMS therapy can be up to $36,000, but insurance coverage can bring that cost down substantially.
The bottom line
Whether used as a standalone treatment or alongside other interventions, TMS is a safe, effective option for OCD, major depressive disorder, anxious depression, adolescent depression, and smoking cessation, with FDA clearance.
Key takeaways
- TMS is FDA-cleared for major depressive disorder, depression with anxiety, migraines, and smoking cessation. For conditions like bipolar depression, postpartum depression, addiction, and PTSD, TMS demonstrates promising outcomes.
- TMS may be more effective than medication or talk therapy alone, with faster results and fewer side effects.
- Results vary depending on the individual and the type of TMS therapy, with SAINT TMS providing the highest remission rate. Fewer TMS centers offer SAINT TMS, with Radial in that exclusive group.
Frequently asked questions (FAQs)
Is TMS safe?
When administered by trained clinicians with proper screening, TMS is a safe treatment for OCD, depression, and other conditions. It has relatively few side effects, most of which only lasts a few minutes, and is low risk.
Is TMS shock therapy?
TMS is not shock therapy. TMS is a non-invasive, painless procedure in which a small electromagnetic coil rests against the scalp and delivers brief magnetic pulses to precise brain regions.
Does TMS therapy work?
According to decades of clinical research, TMS works! Remission rates for depression can be as high as 90% in some patient populations, plus the treatment is safe, non-invasive, and may be used in tandem with talk therapy and other treatment modalities.
What is TMS therapy used for?
TMS is FDA-cleared for major depressive disorder, anxious depression, OCD, migraines, and smoking cessation. It is also being actively studied for a wide range of other conditions, including postpartum depression, bipolar disorder, PTSD, schizophrenia, addiction, Parkinson’s disease, and stroke recovery.
Can I drive after TMS?
Driving after TMS is safe. You can drive yourself to and from the clinic, and many patients return to work or school right after.
What are the side effects of TMS?
Common side effects include mild to moderate scalp discomfort at the treatment site, headache, neck or jaw pain, tinnitus (ringing in the ears), tingling or twitching of facial muscles during stimulation, brief light-headedness, and temporary fatigue. These reactions usually fade within minutes to hours and typically respond to over-the-counter pain relievers. Serious events are very uncommon; the most significant risk is a seizure, occurring in far less than one percent of patients.
How long does TMS last?
A typical TMS session lasts about 3–10 minutes. Accelerated TMS typically consists of 50 sessions over the span of 5 days, or 30 treatments over 5 half-days. Traditional TMS treatment is delivered one or two times a day over the course of 6–10 weeks, depending on your specific diagnosis, protocol, and schedule. At centers like Radial, our doctors personalize treatment to your symptoms and schedule.
How long does TMS take to work?
Many patients begin to notice improvements in their mood after several sessions, though the timeline can vary. Some individuals may experience relief sooner, while others may take a little longer to see significant changes.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




