Types of Depression: From Major to Persistent and Everything In Between
.png)
Depression isn’t just one condition—it’s a spectrum, and no two people go through it in exactly the same way. For some, it takes the form of major depressive disorder, marked by episodes so heavy that getting out of bed feels impossible. For others, it’s a quieter, lingering fog that stretches on for years. But no matter how it shows up, depression is real, valid, and deserving of care.
Many people think of depression as sadness or exhaustion. But the reality is much more complex. Depression is not one-size-fits-all, and understanding the various types of depression can be the first step toward finding relief that actually works.
Clinicians use the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to define and diagnose several official types of depressive disorders. But if you’ve ever searched online for answers, you’ve probably seen other terms too, like “functional depression,” “double depression,” or “depression that comes and goes.” Those words capture real experiences, even if they aren’t always in the textbooks.
This comprehensive guide will walk you through the major types of depression and how they differ, as well as the treatment options that may offer some relief.
What is depression?
Depression is a mental health condition that affects how you feel, think, and function day to day. It’s different from ordinary sadness or the natural grief that comes with loss. Depression lingers, and it can interfere with work, relationships, and daily routines in ways that feel overwhelming. But rest assured, it’s also a condition that can be understood and treated.
Signs of clinical depression include:
- Persistent low mood or emptiness
- Loss of interest or pleasure
- Changes in sleep or appetite
- Fatigue or low energy
- Difficulty concentrating or making decisions
- Feelings of guilt, worthlessness, or hopelessness
- In severe cases, thoughts of death or suicide
“The diagnosis of depression is based on an individual’s report of experiencing particular symptoms for at least several weeks,” says Mark Russ, MD, a psychiatrist and chief medical officer of Silver Hill Hospital in White Plains, New York. “There is no laboratory test, for example, that permits us to make the diagnosis.”

What are the different types of depression?
Depression doesn’t just present in one way—it wears many faces. Some forms are clearly defined in the DSM-5, while other types of depression are named by people who are living through it. However depression shows up, your experience is real and worth paying attention to. Here’s a guide to the most widely discussed types, so you can start to see where your own experience might fit (and how to treat it).
Major depressive disorder (MDD) or clinical depression
Major depressive disorder is the most common and recognized type of depression. It involves experiencing at least one major depressive episode, which is at least two weeks of persistent sadness or loss of interest in everyday activities, along with other symptoms like:
- Changes in sleep
- Changes in appetite
- Lack of energy
- Difficulty concentrating
You can have severe, moderate, or mild depression episodes, and they can happen once or recur throughout life. Here’s a breakdown of MDD’s subtypes.
With anxious distress
This describes depression that comes with a high level of anxiety. It’s common—50 to 75 percent of people with major depression will meet criteria for anxious depression.
Patients with the anxious subtype of depression, will experience most of their anxiety as part of their depressive episode; others suffer from anxiety as a separate and distinct disorder. “A majority of patients diagnosed with depression will also experience anxiety. Patients with depression will not infrequently also meet criteria for an anxiety disorder, including generalized anxiety disorder, panic disorder, agoraphobia, and social phobia,” says Russ. “The diagnosis of a comorbid anxiety disorder is important because it may complicate the treatment of depression.”
When anxiety and depression overlap, symptoms may include:
- Feeling tense, worried, or like something bad will happen
- Feeling like you’re out of control
- Restlessness
If this feels familiar, you’re not alone—and it’s not a sign that recovery is out of reach. It just means treatment may need to address the full range of symptoms. A healthcare provider can help sort through it and find the right plan. A combination of talk therapy and medication often provides meaningful relief for many.
Advanced treatment options are also emerging. For example, the BrainsWay H1 coil was the first FDA-approved device specifically designed to treat anxious depression using deep transcranial magnetic stimulation (TMS).
With mixed features
Mixed features occur when a person shows signs of depression and mania at the same time. For example, someone may feel hopeless, but also experience racing thoughts or bursts of energy. This overlap can sometimes be mistaken for bipolar disorder; the difference is that people with mixed features experience depression with some manic/hypomanic symptoms but never enough to meet criteria for hypomania or mania.
Depression with mixed features can also include symptoms like:
- An overly euphoric mood
- Inflated self-esteem
- Increased energy
- Talking a lot
- Sleeping less
- Taking risks
Unlike many other forms of depression, antidepressants on their own aren’t always the best choice for people with mixed features. In some cases, they can increase the risk of manic symptoms. That doesn’t mean treatment isn’t possible—it just looks a little different.
Doctors may recommend antipsychotic medications or mood stabilizers such as lithium, often alongside therapy. Many will respond to TMS. For some, treatments like electroconvulsive therapy are necessary to bring relief.
With melancholic features
Melancholic depression is defined by a profound loss of pleasure—things that once brought joy or comfort suddenly feel flat or unreachable. It’s more common than many people realize. In one study, nearly 61 percent of the 1,410 depressed people studied had melancholic symptoms alongside their MDD.
These symptoms can include:
- Weight changes
- Loss of pleasure in almost all activities
- Depression that is regularly worse in the morning
- Early-morning awakening
- Excessive or inappropriate guilt
According to the same study, it’s unclear if certain treatments work better for melancholic features than others. But in general, effective options can include medications along with talk therapy. Antidepressants, alone or in combinations, as well as TMS and Esketamine will help most patients.
Atypical depression
Despite the name, atypical depression is fairly common. Its defining trait is mood reactivity, which means that positive events can temporarily improve a depressed mood. In addition to the common symptoms of MDD, other telltale symptoms include:
- Increased appetite or weight gain
- Excessive sleep
- A heavy feeling in the arms or legs
- Strong sensitivity to rejection
The good news is that atypical depression responds to treatment. Psychotherapy, medication, and consistent healthy habits (like regular movement, a nutritious diet, and quality sleep) can all make a meaningful difference.
.png)
Psychotic depression
Psychotic depression happens when delusions or hallucinations accompany severe depression. Signs of psychotic depression include:
- Delusions of guilt, inadequacy, illness, or nihilism
- Derogatory auditory hallucinations
- Difficulty with social interactions
- Motor issues like unintentional motions or restlessness
Because of the added layer of psychosis, this form of depression can be very disabling and requires prompt medical care.
Inpatient treatment is more common with psychotic depression than with other subtypes of MDD, since it provides safety and stabilization. Experts typically recommend a combination of antidepressant and antipsychotic medications.
However, when psychotic depression is marked by somatic delusions—such as false beliefs about illness or body dysfunction—electroconvulsive therapy (ECT) tends to work especially well, while second-generation antipsychotics are often less effective. In many cases, ECT can bring significant relief when other treatments have not. The important thing to know is that recovery is possible with the right combination of support and treatment.
Catatonic depression
Catatonic depression is rare but serious. Experts aren’t sure what causes it, though it’s also associated with other mental health conditions like bipolar disorder and schizophrenia. Catatonic depression involves disturbances in movement and behavior, such as:
- Staying immobile for long periods, sometimes in an uncomfortable position
- Resisting attempts to change their position
- Lack of reactions
- Agitation
- Refusing to speak
- Mimicking others’ sounds or movements
- Grimacing
- Making repetitive, purposeless movements
- In severe cases, life-threatening complications like dangerously high body temperature, heart rate, and blood pressure
Catatonic depression can also be life-threatening if not treated. In severe cases, patients stop eating or moving, which can lead to dehydration or blood clots (deep vein thrombosis). In the most critical cases, dangerous spikes in body temperature, heart rate, or blood pressure can occur.
Treatment often involves benzodiazepine medications (such as lorazepam) in addition to antidepressants. When symptoms are severe or do not respond to medication treatment, electroconvulsive therapy (ECT) can provide rapid relief, sometimes with significant functional improvement after the very first treatment. With prompt care, people with catatonic depression can and do recover.
Prenatal depression
Prenatal depression develops during pregnancy and may be the result of genetics, hormonal shifts, or the physical, financial, and mental stressors that come with preparing for a baby. Common signs include:
- Anxiety
- Changes in appetite and weight
- Irritability or depressed mood
- Excessive mood swings
- Loss of interest in sex
- Difficulty connecting with your partner
Because it occurs during such a vulnerable time, prenatal depression can feel especially isolating. But support is available, and treatment is safe for both parent and baby. Cognitive behavioral therapy, interpersonal therapy, and psychotherapy can help ease symptoms and strengthen coping strategies. In some cases, medication may also be helpful.
Postpartum depression
Postpartum depression occurs after childbirth and goes far beyond the “baby blues.” While many new parents feel mood swings or fatigue in the first weeks, postpartum depression is longer-lasting, more severe, and quite disabling. It affects up to 15 percent of people after giving birth and can last for weeks or months without treatment.
Symptoms may include:
- Waves of sadness and hopelessness
- Crying for no reason
- Difficulty bonding with or not wanting the baby
- Feeling completely overwhelmed around your baby
- Thoughts of hurting your baby or yourself
- Psychosis
The exact cause isn’t clear, but it may be related to a sudden drop in hormones combined with the intense physical and emotional demands of new parenthood. Therapy and medication are effective treatments, and in more severe cases, electroconvulsive therapy may be considered.
Seasonal affective disorder (SAD)
Seasonal affective disorder is a type of depression that occurs seasonally, usually starting in late fall or winter when daylight hours are shorter. The lack of sunlight can affect mood-regulating brain chemicals, hormones, and vitamin D levels, leading to symptoms such as:
- Cravings for carbohydrates
- Weight gain
- A heavy feeling in the arms or legs
- Anxiety
- Agitation
- Oversleeping
- Thoughts of death or suicide
Treatment for SAD often includes the same options used for other types of depression, such as therapy and medication, but also has some targeted approaches. Spending time outside during daylight hours, using a light therapy lamp, and taking vitamin D supplements are all proven strategies. For many, these steps can ease symptoms and restore balance until the seasons shift again.
Treatment-resistant depression (TRD)
Treatment-resistant depression describes cases where standard treatments, like antidepressants, have not provided enough relief. It affects about 30 percent of people with MDD, and symptoms often feel more intense or harder to shake. TRD can lead to:
- Longer depressive episodes
- Anxiety
- Thoughts of suicide
- More severe depressive symptoms overall
Needing more than first-line treatments doesn’t mean you’re out of options. While some people with treatment-resistant depression find benefit in switching or combining antidepressants, others improve with advanced therapies. These include transcranial magnetic stimulation, esketamine (Spravato) nasal spray, and electroconvulsive therapy. At Radial, we specialize in offering these kinds of interventional treatments, designed to help when traditional paths haven’t worked.
Persistent depressive disorder (PDD)
Persistent depressive disorder, also called dysthymia or chronic depression, is a long-lasting form of depression that about 1.5 percent of U.S. adults experience each year.
Unlike major depressive disorder, which comes in more distinct and often more severe episodes, PDD involves a continuous low mood that lasts for two years or longer in adults (or at least one year in children and teens), says Stephanie Hartselle, MD, a psychiatrist and clinical associate professor at Brown University.
The symptoms may not always feel as intense as those of major depression, but because they stretch on for such a long time, they can be just as disruptive. Many people with PDD describe it as living under a constant gray cloud. Daily life may continue, but the ability to feel joy or motivation is dulled. Because symptoms can become part of someone’s “normal,” it sometimes goes undiagnosed.
Treatment for PDD often includes talk therapies such as cognitive behavioral therapy or interpersonal therapy, which help shift negative thought patterns and build healthier coping strategies. Antidepressants can also be helpful, especially when combined with therapy.
Double depression
Double depression occurs when a person with persistent depressive disorder experiences a major depressive episode on top of their chronic low mood. In these cases, symptoms suddenly become much more severe, often leading to greater impairment and distress.
Without treatment, double depression can last longer and be harder to recover from than either condition on its own. But recovery is possible. The most effective approach usually combines psychotherapy with medication, addressing both the long-standing baseline of depression and the acute episodic depression layered on top. In cases of non-response to conventional antidepressants, Esketamine and TMS can be effective alternatives.
Functional depression
Functional depression is not an official diagnosis. Instead, it’s “the idea that colleagues, friends, and even family may not know how much someone is suffering from their depression, as they can still occupationally perform or appear relatively normal in social settings,” says Harselle.
For instance, a person with functional depression might keep up with work deadlines, maintain relationships, or manage household responsibilities, all while feeling persistently sad, drained, or unmotivated inside.
Because the outward signs are less visible, this type of depression often goes unnoticed by others, and sometimes even by the person experiencing it. This can delay recognition and treatment. The good news is that functional depression responds to the same treatments as other forms of depression: therapy, medication, and supportive lifestyle changes can all help restore energy and hope.
Premenstrual dysphoric disorder (PMDD)
Premenstrual dysphoric disorder, or PMDD, is a severe form of premenstrual syndrome (PMS). While PMS can cause mood swings, bloating, or irritability in the days leading up to a period, PMDD goes further. It involves intense mood-related symptoms that interfere with daily life, work, or relationships, says Harselle.
Common PMDD symptoms include:
- Severe irritability or anger
- Brain fog
- Extreme mood swings
- Feelings of hopelessness, sadness, or overwhelm
- Anxiety and panic attacks
- Trouble concentrating
- Sleep problems
- Physical symptoms like breast tenderness, bloating, or headaches
The key difference between PMS and PMDD is severity. PMS may be uncomfortable, but PMDD is disabling for many people. Symptoms often kick in about a week before menstruation, improve once bleeding starts, and are absent the rest of the month (though some people experience longer or shorter periods of PMDD).
Doctors may diagnose PMDD by asking patients to track their symptoms over several cycles. Treatments often include antidepressant medications (especially SSRIs), birth control pills or hormonal therapy, and lifestyle strategies like regular exercise and stress management. Cognitive behavioral therapy can also help with coping.
Disruptive mood dysregulation disorder (DMDD)
Disruptive mood dysregulation disorder is a diagnosis given primarily to children and adolescents. It is characterized by severe, frequent temper outbursts—verbal or physical—that are out of proportion to the situation. Between outbursts, children with DMDD often have a persistently irritable or angry mood, making it hard to function at home, at school, or with peers.
To meet diagnostic criteria, these symptoms must:
- Occur three or more times per week
- Last for at least 12 months
- Be present in more than one setting, such as at home, school, or with peers
DMDD is usually diagnosed between the ages of 6 and 10. Treatment can include a combo of behavioral therapy, parent training, and school support. In some cases, medications such as antidepressants, stimulants, or mood stabilizers may be used to help manage symptoms.
Depressive disorder due to another medical condition
Sometimes depression develops as a direct result of another medical problem. This is known as depressive disorder due to another medical condition. In these cases, depression is not simply a reaction to being sick—it’s caused by changes in the body related to the illness itself.
Medical conditions that may trigger depression include:
- Neurological disorders like Parkinson’s disease, multiple sclerosis, or stroke
- Endocrine disorders such as hypothyroidism or Cushing’s disease
- Chronic illnesses like cancer, heart disease, or diabetes
- Certain infections or immune conditions
The symptoms often look very similar to those of major depression, but the root cause is different. For example, a thyroid disorder can directly affect the hormones that regulate mood. In these cases, treatment typically involves addressing both the underlying medical condition and the depression. That may mean medical management of the illness alongside therapy, antidepressant medication, or other supportive care. With the right approach, symptoms can improve on both fronts.
Bipolar I and II disorders
Bipolar disorders are not classified as depressive disorders, but they include episodes of depression that can be just as severe—or even more disabling—than those seen in major depressive disorder. Though the depressive symptoms are similar to MDD, the main difference is that people with bipolar disorder also have periods of mania or hypomania.
Here are the subtypes:
- Bipolar I disorder involves at least one manic episode. Symptoms can include an abnormally elevated or irritable mood, increased energy, decreased need for sleep, and risky or impulsive behavior. Depressive episodes are also common and can be long-lasting.
- Bipolar II disorder involves hypomanic episodes, which are less intense than full mania, along with significant depressive episodes. Hypomania may look like high energy or productivity, but the depressive episodes often cause the most impairment.
Treating bipolar depression requires special care. Antidepressant medications on their own can sometimes trigger mania or worsen mood cycling, so doctors typically prescribe mood stabilizers such as lithium or lamotrigine, atypical antipsychotics, or a carefully balanced combination. TMS is another safe and effective treatment option, while ECT is reserved for severe or difficult-to-treat cases. Psychotherapy, lifestyle adjustments, and steady routines also play a crucial role in managing symptoms.
In addition to medical treatment, the awareness of loved ones can play a key role in recognizing early shifts in mood and ensuring timely care.
“Having a family member with bipolar disorder means if I am noticing subtle signs something is off (like more irritability over little things), I have learned to trust my instincts and let my partner know what I’ve observed,” says Carlene MacMillan, MD, whose partner has bipolar disorder. “It’s like they say on the NY subway: ‘If you see something, say something!’ Loved ones are often the first to notice subtle changes in mood episodes, including early signs that a treatment is working.”
Cyclothymic disorder
Cyclothymic disorder, also called cyclothymia which is a subtype of cyclical depression, is a milder but long-term form of bipolar disorder.
“It describes episodes over two or more years that involve depressive symptoms that fall short of MDD, and periods of hypomania, a less severe form of mania that’s shorter in duration,” says Harselle. In other words, these shifting moods don’t meet the full criteria for major depression or bipolar disorder.
People with cyclothymia often describe it as living with moods that rise and fall in waves, like depression that comes and goes without ever fully settling. For a diagnosis, symptoms need to persist for at least two years in adults (or one year in children and teens), with no stretch of stable mood lasting longer than two months.
Depressive symptoms are similar to those of major depressive disorder, while hypomanic periods may bring:
- Increased energy
- Reduced need for sleep
- Talkativeness
- Irritability
Although cyclothymia can feel less severe than bipolar I or II, the ongoing fluctuations can still take a toll on relationships, work, and self-esteem. Treatment often involves mood stabilizers or atypical antipsychotic medications, along with psychotherapy to strengthen coping skills. Consistent routines and healthy habits can also make mood swings easier to manage.
Situational depression
Situational depression, also known as adjustment disorder with depressed mood, develops in response to a stressor. Unlike major depression, which can occur at random, situational depression involves “a triggering event like a breakup, the death of a loved one or pet, job loss or other situational stressor,” says Harselle. “This can result in depression that may not meet criteria for MDD, but is still incredibly impactful.”
Along with the typical symptoms of major depressive disorder, symptoms of situational depression can include:
- Sadness or tearfulness
- Loss of interest in normal activities
- Sleep problems
- Feeling overwhelmed or difficulty coping
The condition usually appears within three months of the triggering event and tends to resolve once the stressor improves or the person adjusts. For most people, situational depression lasts less than six months, but if the stressor continues, symptoms can persist for several years, says Harselle.
Treatment often focuses on short-term support. Treatment may involve short-term psychotherapy, such as cognitive behavioral therapy, to help develop healthier coping strategies and reduce distress. In some cases, temporary use of antidepressant or anti-anxiety medications can also help people regain balance.
When to seek help—and where to start
No matter what level of depression you’re living with, it’s important to remember that depression is treatable. Even if you’ve carried symptoms for years or feel like you’ve “tried everything,” there are still options for recovery. The first step—reaching out for support—can feel daunting, but it’s also the most powerful.
If you see yourself in any of the descriptions above, start by talking with a primary care provider or a mental health professional. You don’t need to walk in with all the answers or know exactly which type of depression you have. Your provider can help piece together your symptoms, medical history, and life context to arrive at the right diagnosis and treatment plan.
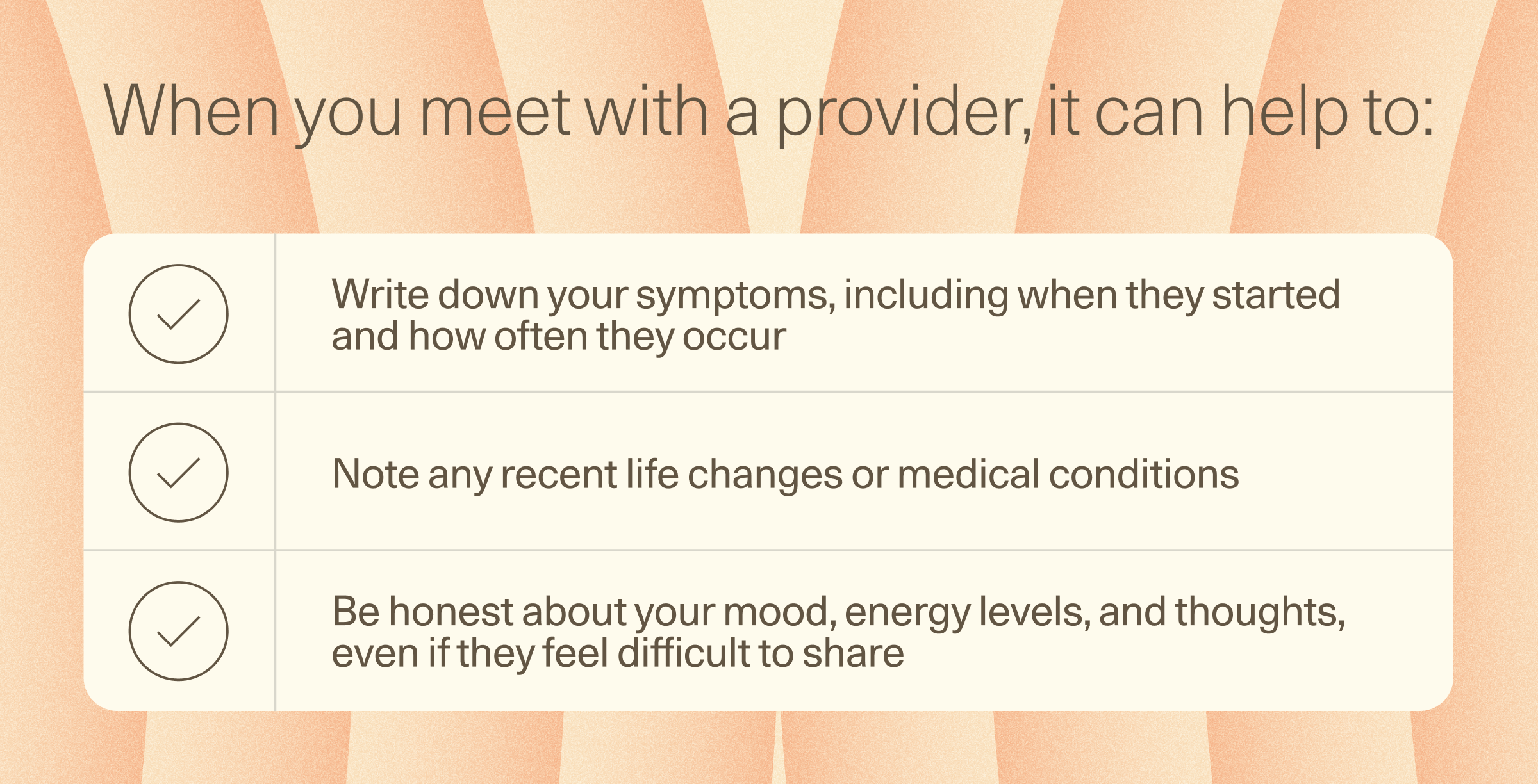
When you meet with a provider, it can help to:
- Write down your symptoms, including when they started and how often they occur
- Note any recent life changes or medical conditions
- Be honest about your mood, energy levels, and thoughts, even if they feel difficult to share
For many people, treatment begins with therapy, medication, or both. But if you’ve already tried traditional approaches and still don’t feel relief, you’re not out of options. At Radial, we offer treatments such as transcranial magnetic stimulation, Spravato, and PRISM neurofeedback therapy, which can provide hope for people with treatment-resistant depression or those looking for alternatives to medication.
The bottom line
Living with depression can feel isolating, but support and effective treatments are within reach. If traditional care hasn’t helped, innovative options like TMS, Spravato, or PRISM neurofeedback may offer new hope. With the right approach, symptoms can ease and real relief is possible. Taking the first step to reach out can open the door to healing.
Key takeaways
- Depression isn’t one-size-fits-all—it comes in many forms, from major depressive disorder to persistent low mood, seasonal patterns, and hormonally-driven shifts.
- Recognizing the type of depression you’re experiencing can help guide more effective treatment and give language to what you’re going through.
- All forms of depression are treatable, even if symptoms have lasted for years or haven’t improved with first-line treatments.
- Care can include therapy, medication, lifestyle changes, and advanced options like transcranial magnetic stimulation, Spravato, or PRISM neurofeedback therapy.
Frequently asked questions (FAQs)
What are the types of depression?
There are several recognized types, including major depressive disorder (MDD), persistent depressive disorder (PDD), seasonal affective disorder (SAD), perinatal depression (prenatal and postpartum), premenstrual dysphoric disorder (PMDD), and treatment-resistant depression. Other terms people often use—like functional depression or double depression—describe real experiences even if they aren’t official diagnoses.
What triggers a depressive episode?
Triggers differ from person to person. Stressful life events, trauma, seasonal changes, hormonal shifts, and underlying medical conditions can all play a role. Sometimes, depressive episodes happen without a clear external cause due to changes in brain chemistry or genetics.
What is the hardest type of depression?
There isn’t one definitive “hardest” type, since the level of depression and the range of disabling symptoms depend on the individual. That said, treatment-resistant depression, psychotic depression, and catatonic depression are often considered especially challenging because of their intensity and impact on daily life.
Can you have more than one type of depression?
Yes. It’s possible to experience overlapping types—for example, someone with persistent depressive disorder may also go through a major depressive episode (“double depression”). Others may have depression along with anxiety or another mental health condition.
How long can depression last?
It varies. A single depressive episode may last a few weeks to several months, while persistent depressive disorder can stretch on for years. The good news is that all types of depression are treatable, and with the right support, symptoms can improve.
Deep dive recommendations
- The Frontier Psychiatrists. The Scalable Depression Solution.
- Pscyhofarm Podcast. The Deficit Model & Difficult to Treat Depression Featuring Dr. Chris Aiken.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




