Does Ketamine Therapy Get You High? Separating Fact From Fear
.jpg)
Does ketamine therapy get you high? The answer is nuanced, and understanding it could reshape how you think about mental health treatment.
Honestly, when I first heard about it, I wondered the same thing. And I consider myself pretty open-minded—I’m a trained social worker and a mental health writer—but the only images I could conjure were hazy flashbacks of rave culture and whispered stories about “K-holes.” How could something I’d once heard called a party drug possibly be safe, let alone healing?
Turns out, context is everything. In carefully monitored doses, ketamine may open new doors in the brain that can help people struggling with conditions like treatment-resistant depression, PTSD, and more. In fact, ketamine treatment for depression has shown promise where standard medications fall short, offering relief to people who’ve tried just about everything else.
This article will unpack what ketamine therapy actually feels like, why those sensations happen, how it differs from recreational use, and whether it’s addictive. The goal? To clear up the myths, calm some of the fears, and give you the science-backed info you need to decide if this treatment is worth exploring—for yourself or someone you love.
What is ketamine therapy?
Once just an anesthetic in the operating room, ketamine is now making waves in mental health care and other areas of medicine like pain management. Research shows it may help with conditions like:
- Depression
- Suicidal thoughts
- Post-traumatic stress disorder (PTSD)
- Certain chronic pain conditions (including migraine and fibromyalgia)
- Early data also suggests ketamine therapy may be useful in treating obsessive compulsive disorder (OCD) and substance use disorders
Ketamine therapy has generated particular buzz as a potential treatment for treatment-resistant depression. Depression changes how brain cells talk to each other. Unlike traditional antidepressants, ketamine therapy for depression works on a completely different system in the brain and seems to spark regrowth of lost connections. That may be why it often works for people who haven’t found relief from standard meds.
Ketamine can be delivered in several ways: intravenously (IV), by intramuscular injection, orally (as a tablet), or as a nasal spray. IV is often considered the gold standard since it’s 100% bioavailable.
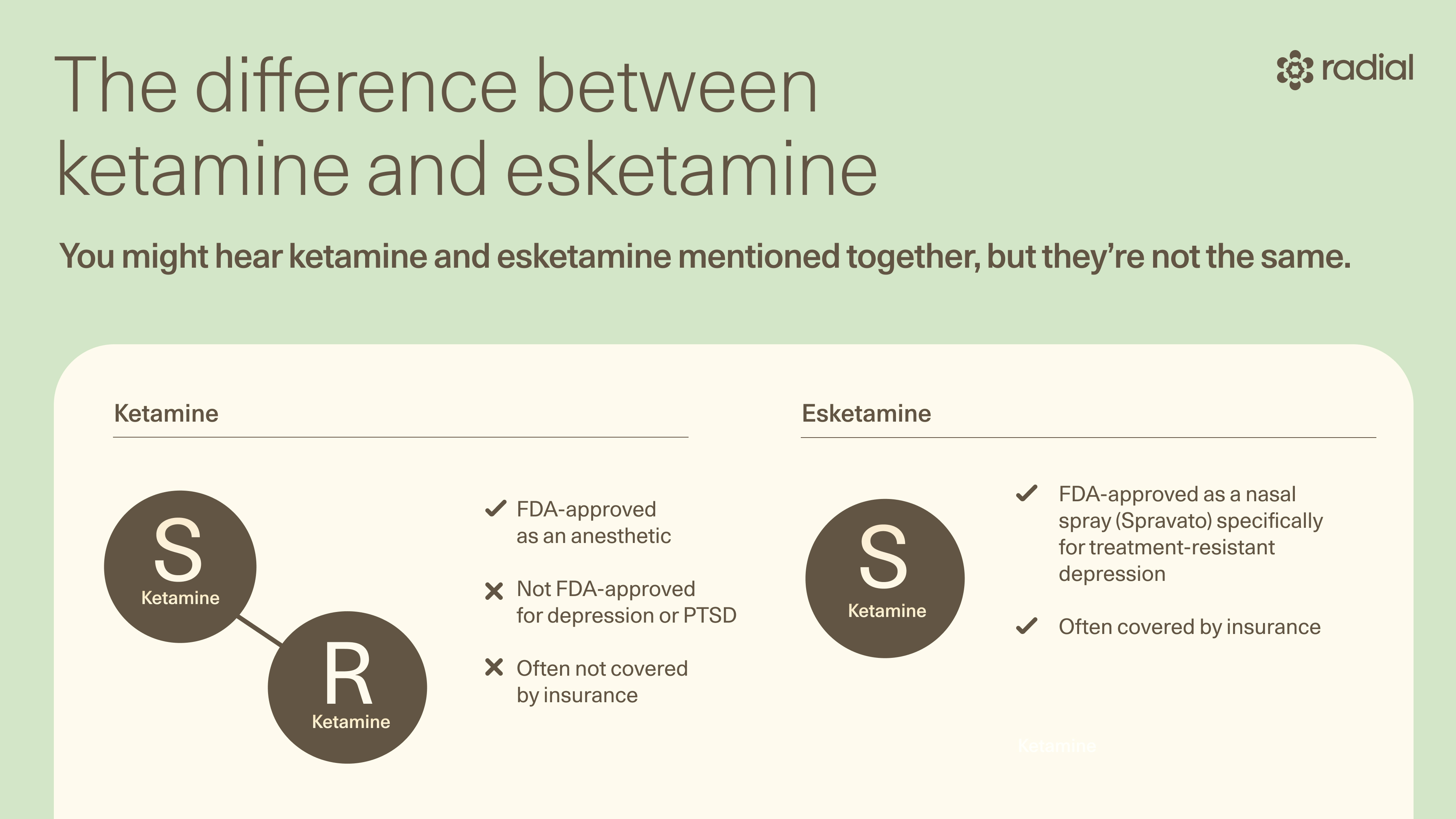
You’ll also hear about esketamine, but it’s not exactly the same thing. Ketamine has two molecules (R- and S-ketamine) while esketamine contains just the S form. That tiny chemical tweak changes how your body processes the drug and how the FDA regulates it.
Here’s the catch: ketamine-assisted therapy for mental health is considered “off-label.” In other words, while the FDA has approved ketamine as an anesthetic, it hasn’t received an official stamp of approval for depression, PTSD, or other mental health uses. Because of that, insurance usually won’t cover it.
Esketamine, however, is FDA-approved as a nasal spray (brand name Spravato) for treatment-resistant depression, which means it’s more likely to be covered by insurance.
Does ketamine therapy get you high?
Let’s get this out of the way: yes, ketamine can make you feel altered. It has psychoactive properties, meaning it can create a sense of detachment from reality or mild distortions of time and space, or what some might call feeling “high.”
But no two experiences are alike. How people feel on ketamine varies a lot from person to person, says Ahmed Tahseen, MD, clinical advisor at Radial, medical director at Biohaven Therapeutics, and clinical instructor of psychiatry at Yale University. “The mind-altering effects peak within a few hours, then taper off, though some people notice lingering shifts in mood for a few days to a week.”
How the experience feels also depends on how it’s delivered. In Dr. Tahseen’s clinical experience, IV and intramuscular routes tend to feel the most potent. Patients and providers often prefer intramuscular because they believe the dose can be more easily adjusted to individual needs, he says. On the flip side, some say oral or nasal routes create a subtler, less intense effect, he explains.
If you’re new to ketamine, it’s best to go in with an open mind since your response may not match what you’ve heard from others, adds Dr. Tahseen.
And while ketamine’s psychedelic effects have given it a reputation as a party drug, therapy is a completely different ballgame. In a clinical setting, dosing is carefully controlled for safety, and ideally, you’re working with a therapist before, during, and after the session to process the experience, says Dr. Tahseen. All this to say, ketamine therapy is not about chasing a high, but about creating space for healing.
The science of the “high”
So what’s actually happening in your brain when ketamine makes you feel floaty, trippy, or “out of body”? Scientists are still piecing it together.
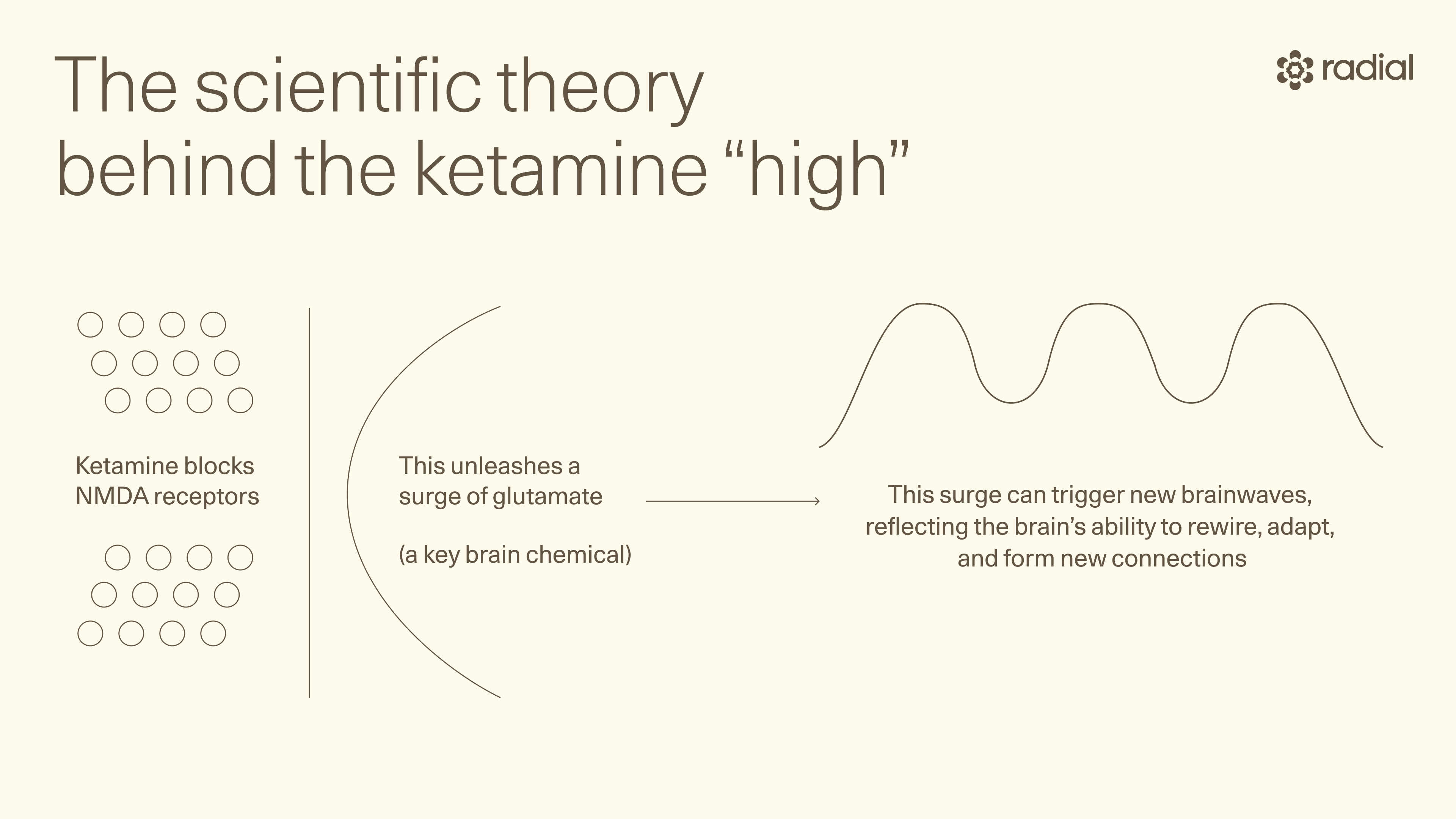
Research shows ketamine can trigger new oscillation patterns (brainwaves) in areas like the posteromedial cortex (a part of the brain thought to produce its psychedelic effects). The leading theory is that these oscillations happen when ketamine blocks NMDA receptors, which unleashes a surge of glutamate (a key brain chemical), says Dr. Tahseen. This surge then activates AMPA receptors, which are tied to neuroplasticity—your brain’s ability to rewire, adapt, and form new connections.
But here’s the twist: this is probably not the whole story. “Most medications we use affect dozens of receptors in ways we know and many more that we do not,” says Dr. Tahseen. With SSRIs, for example, serotonin reuptake inhibition may explain only a fraction of their impact. The rest? Still a mystery. Ketamine is no different.
Even the NMDA theory has cracks. For years, experts believed NMDA receptor antagonism only caused psychosis, says Dr. Tahseen. Then ketamine surprised everyone by easing depression in some patients, forcing scientists to rethink the mechanism. But when other drugs with the same action didn’t deliver the same antidepressant benefits, that theory began to wobble—or at least it doesn’t appear to paint the whole picture about how ketamine works, he says.
Many believe that the psychedelic effect is not necessary for the beneficial effect of ketamine. But nevertheless, there is a lot to be learned. Some evidence suggests different brain regions may be responsible: the dissociative, sensory effects might stem from the posteromedial cortex, while the mood boost may come from another (like the prefrontal cortex and hippocampus).
“The real answer is: we don’t know,” says Dr. Tahseen. What we have now are a lot of theories and educated guesses, he says. In other words, the science is still catching up, and what we understand today may only scratch the surface of how ketamine impacts the brain and a person’s experience while using it.
Make no mistake: a therapy session and a party high are two totally different worlds. Let’s break down what makes the clinical experience of ketamine so different from recreational use.
Intent
Here’s the thing: why you take ketamine changes how you experience it. At a party, it’s usually about an escape. In therapy, people come in with the intent to heal, and that makes all the difference.
In clinical settings, ketamine’s antidepressant effects are much more likely to show up than in recreational use, says Dr. Tahseen. Why? Part of it may be having a goal to heal. When we set an intention to get better, a cascade of psychological and neurobiological effects unfold, explains Dr. Tahseen.
Setting a “positive intention at the beginning of each treatment” can “optimize the therapeutic benefit,” agrees MaryEllen Eller, MD, a board-certified adult psychiatrist.
Safety
Safety and trust also play a huge role. When people believe their doctor can “facilitate a safe experience” and guide them through difficult moments, they’re more open to exploring vulnerable emotions that otherwise stay buried, says Dr. Tahseen. “We have tremendous unconscious defenses that do not allow the vulnerable things about us to be seen when we do not believe we are safe,” he explains.
Ketamine treatment also follows a safety protocol that partying doesn’t. When ketamine is taken under the supervision of a mental health professional and accompanied by psychotherapy, there’s preparation before the process, support during the session, and help to integrate the experience afterward, says Dr. Tahseen. “Understanding the process ahead of time can decrease anxiety and improve the experience,” adds Dr. Eller.
In recreational settings, you don’t usually have a therapist sitting nearby to help you process what comes up. That absence alone makes the experience vastly different.
Dose
On the dance floor, there’s no measuring cup. Doses can run high, and with that come risks: temporary psychosis-like symptoms, cognitive impairment, and even lasting psychological issues when used heavily over time.
In therapy, the approach is the opposite—low, precisely measured doses delivered by trained professionals. Whether administered by IV, injection, nasal spray, or orally, you know exactly what’s entering your system and why. That level of control is a large part of what makes medical ketamine use safer.
Side effects and risks
Recreational ketamine can be dangerous:
- It can result in ketamine poisoning, especially when mixed with other substances
- Combined with alcohol or opioids, it can cause blackouts, vomiting, or even fatal overdoses
- Paired with other hallucinogens like LSD or mushrooms, the risks of disorientation and accidents skyrocket
- Higher doses can trigger severe, schizophrenia-like effects, and long-term heavy use may lead to lasting neuropsychiatric issues like cognitive decline and poor mental health
In clinics, side effects like upset stomach, dizziness, temporary confusion, and elevated blood pressure are still possible. The difference? You’re in a tightly monitored environment with strict dosing and emergency protocols. A reputable clinic has trained staff and safety equipment (like emergency medications and even a crash cart) on standby in case something goes wrong—not exactly what you’ll find at someone’s loft party.
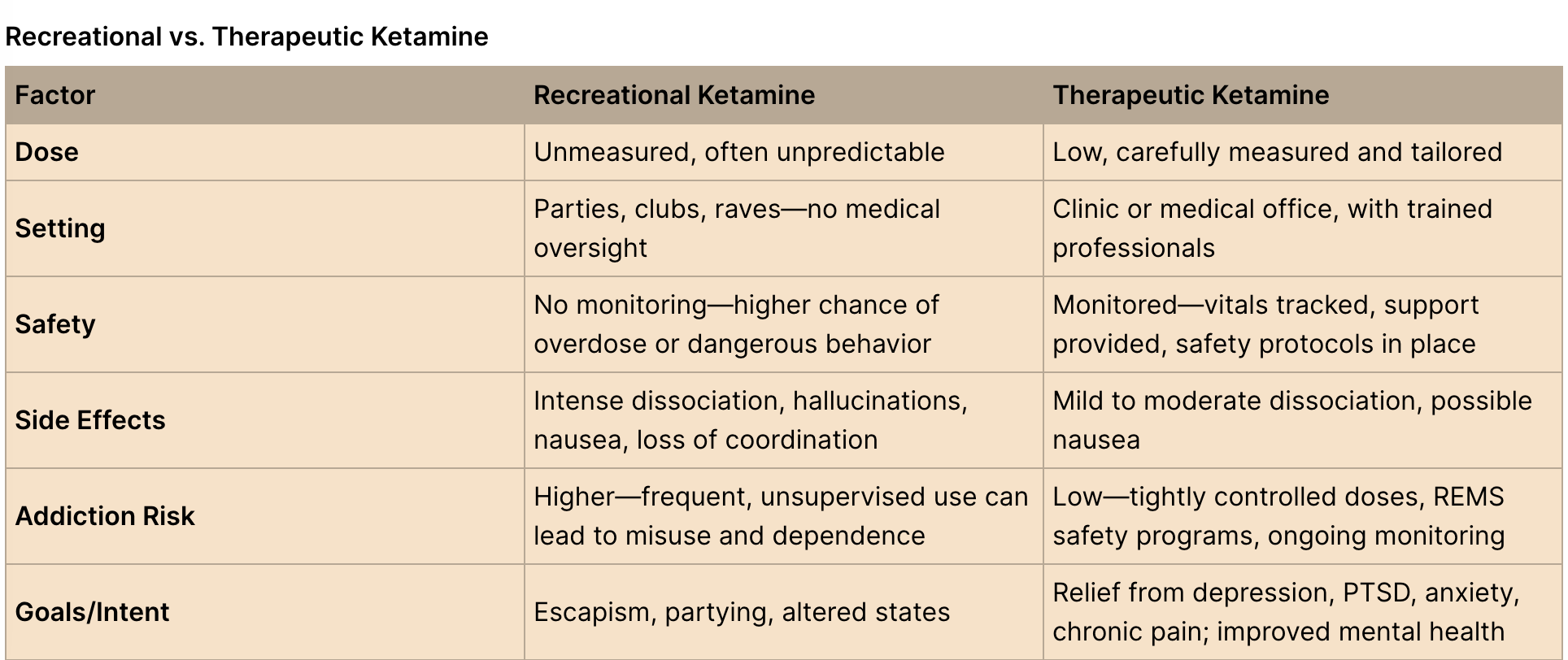
Potential for abuse and addiction
“Recreational ketamine carries a risk of abuse and addiction for a small minority of people,” says Dr. Tahseen. Frequent, heavy use has been linked to withdrawal, risky behaviors, and using more despite knowing the harm. Over time, this can lead to serious emotional and behavioral issues, he says.
But therapeutic use tells a different story. The same potential for addiction “has not translated to ketamine when used as a medicine in a clinical context,” says Dr. Tahseen. Research shows that when ketamine is given in low, controlled doses for a set treatment period, the risk of addiction is much lower (though not zero). The safety protocols and medical oversight make all the difference.
A note on clinic safety: not all practices are created equal
Even in medical settings, ketamine is not automatically safe just because you’re in a clinic. “There are more clinics I would not go to than those I would,” warns Dr. Tahseen. Since ketamine is largely prescribed off-label, the field is largely unregulated, many clinics operate on a cash-only basis, and not all provide the therapeutic support patients need, he explains.
What to look for, according to Dr. Tahseen, is a clinic that:
- has psychiatrists and therapists on staff.
- conducts thorough evaluations (one to three visits) to prepare you for the process.
- provides integration sessions afterward (one to three visits) to help you make sense of the experience and move forward.
Bottom line: be skeptical, ask questions, and lean on trusted referrals, says Dr. Tahseen. The best clinics treat ketamine as a “companion to therapy,” not the main act, he adds.
What ketamine therapy feels like
Curious what actually happens during a ketamine session? Dr. Eller walks us through an esketamine treatment from start to finish:
- Check-in: You’ll empty your bladder (trust us, you won’t want to stumble to the bathroom later when you’re feeling a little uncoordinated) and get your blood pressure checked.
- Set the scene: Get comfy in the treatment area, maybe push play on a calming playlist, and set an intention to help focus the experience.
- Medication is administered:
- 0–15 minutes: the effects usually start—this is the transition into dissociation.
- Around 40 minutes: the experience peaks, and staff will recheck your blood pressure.
- By 120 minutes: the dissociation begins to fade, and your BP gets checked again.
- Wrap-up: Once you’re steady, you’ll leave with your driver (you can’t drive the rest of the day).
So, what does it actually feel like? Sensations may include:
- A sense of detachment from your body or surroundings (aka dissociation)
- Distorted perception of sound, light, or time
- A dreamlike calm, sometimes paired with euphoria
More vividly, some describe the “ketamine feeling” as:
- Heavy, whole-body tingling or numbness
- Feeling like they’re inside a movie or dream
- Floating weightlessly
- A deep wave of relaxation or calmness
- Watching themselves from outside their body
That said, not everyone finds ketamine dreamy. Dissociation can feel anxiety-inducing or unsettling—especially if you’re someone who struggles with PTSD or high-anxiety, says Dr. Eller. “Dissociation by nature can be disorienting and feel like losing control,” she says. That’s why being in a “monitored, safe setting with trained professionals who can provide reassurance is critical for positive outcomes,” she adds. Providers are there to ground you and help you work through anything that surfaces.
All this to say, there’s no one-size-fits-all ketamine experience. Your age, body type, dosage, and even your mindset going in all shape how it feels. Some float away calmly, others wrestle with unease—but both are valid. And in the right therapeutic setting, even discomfort can open the door to healing.

Is ketamine therapy addictive?
The short answer: it can be, but context matters. Recreational ketamine use does carry a risk of abuse and addiction, says Dr. Tahseen. In fact, studies show regular users can develop classic signs of addiction: taking more than intended, chasing the high despite negative consequences, spending lots of time obtaining or using it, or building tolerance (needing more for the same effect).
Here’s the good news: when ketamine is given in a clinical setting at carefully monitored, low doses, the addiction risk appears to be low. Some research even suggests ketamine isn’t universally “liked” or craved by patients with treatment-resistant depression though other studies still raise questions about its addictive potential (even at smaller doses).
But built-in safety checks make a big difference in the clinical context. Take esketamine, for example: it’s only available through a strict FDA program called REMS (Risk Evaluation and Mitigation Strategy). Translation: you can’t just take the nasal spray home. It must be administered under supervision in a clinic to help ensure the benefits outweigh the risks.
In a clinic, medical professionals are watching closely. Providers can evaluate each patient’s individual risk, monitor for red flags of misuse, and adjust treatment if needed. That medical oversight acts as a safety net, helping minimize risks while maximizing benefits.
The takeaway: While recreational ketamine can be addictive, medical ketamine therapy—with supervision and safeguards—has a much lower risk profile.
The bottom line
Ketamine isn’t just a club drug repurposed for the doctor’s office—it’s a powerful, fast-acting option for people who haven’t found relief with traditional treatments. While it can spark altered states or feelings of detachment, its therapeutic potential goes deeper, helping rewire brain connections linked to mood. That said, it’s not a one-size-fits-all fix. The right dose, delivery method, and setting matter—a lot.
If you’re curious whether ketamine therapy might be right for you, don’t go it alone. The experts at Radial can help you cut through the noise, weigh your options, and access evidence-based treatments safely. Connect virtually or in person with a licensed clinician who’ll listen, understand your needs, and create a personalized plan to help you feel like yourself again.
Key takeaways
- Ketamine is a dissociative anesthetic with unique hallucinogenic and therapeutic effects.
- In controlled, low doses, ketamine therapy can ease depression, suicidal thoughts, PTSD, and certain chronic pain conditions.
- The “high” from ketamine (dissociation, altered perception) is temporary and feels different for everyone.
- Clinical ketamine is carefully monitored for safety—unlike recreational use, which carries higher risks of side effects, overdose, and addiction.
- Esketamine (a related nasal spray) is FDA-approved for treatment-resistant depression and more likely to be covered by insurance.
Frequently asked questions (FAQs)
Is ketamine an opioid?
No. While ketamine and opioids can both ease pain and promote relaxation, they’re not the same thing. Ketamine is a dissociative anesthetic with some hallucinogenic effects—not an opioid. The difference comes down to how they work in the brain: ketamine binds to NMDA receptors while opioids bind to opioid receptors. Sometimes these receptors sit side-by-side, which means they can “cross-talk” a bit (think static on a phone line). But that overlap doesn’t make ketamine an opioid.
What is ketamine used for?
Ketamine started out as a surgical anesthetic, but its resume has expanded. Today, it’s being used and studied for:
- Depression
- Suicidal thoughts
- Post-traumatic stress disorder (PTSD)
- Certain chronic pain conditions (like migraine and fibromyalgia)
- Obsessive compulsive disorder (OCD) and substance use disorders
Does ketamine infusion cause hallucinations?
In some cases, yes. Ketamine can alter how you see, hear, or feel things—sometimes leading to hallucinations. These perceptual shifts are part of its psychoactive profile.
How long do the effects last?
The mind-bending effects usually kick in fast—often within 40 minutes, depending on the delivery method. With esketamine (the nasal spray), the sensations usually start within the first 15 minutes, and peak dissociation happens around the 40-minute mark, says Dr. Eller.
The “trippy” part typically fades within two hours, but the mood-boosting benefits can last much longer—sometimes up to a week. Some research suggests repeated, intermittent infusions may build on these effects and deliver more lasting relief than a single session.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




