Neurofeedback Therapy: What It Is and Who It’s For

While many people can feel improvement in their mental health through lifestyle improvements, talk therapy, and medication, for many people this is not enough—especially in cases of post-traumatic stress disorder (PTSD), depression, and anxiety. That’s where neurofeedback therapy comes in. This safe, drug-free, noninvasive treatment helps people to train their brain to improve their mental or cognitive function; it can also help you manage conditions like migraines, epilepsy, and traumatic brain injuries (TBI). Here’s everything you need to know about the innovative therapy.
Being my mother’s caregiver following her traumatic brain injury (TBI) meant accompanying her to numerous doctor’s appointments and various types of therapy. Out of all her appointments, there was only one she looked forward to each week: neurofeedback therapy. Neurofeedback therapy is a non-invasive, drug-free type of biofeedback which measures brain activity in real-time. It provides a feedback signal to help people train their brain to improve its function.
My mother’s healthcare team had recommended that she try neurofeedback therapy to help alleviate some of the cognitive symptoms of her TBI, like language difficulties, slower mental processing, and difficulty with memory and concentration. But her doctors were especially enthusiastic about the treatment because she also lived with depression and PTSD, both of which had gotten worse since her TBI. Those were also the conditions that improved the most throughout the course of her treatment. She left each session feeling calmer, more at ease, and more optimistic about her recovery.
In addition to depression, PTSD, and TBIs, neurofeedback shows promise as a treatment for ADHD, anxiety, sleep issues, and other conditions. In this article, we'll explain how it works and who it helps, as well as the benefits, costs, safety, and limitations of the treatment.
What is neurofeedback therapy?
Neurofeedback—also known as neurotherapy treatment—is a non-invasive therapeutic intervention that uses electrical sensors on the scalp to monitor brainwave activity. Patients see their neurological activity in real-time on a computer screen, which allows them to learn to modify their brainwave activity by “training” it to respond better and more efficiently.
Dr. Aron Tendler, diplomate of the American Board of Psychiatry and Neurology, says neurofeedback “uses a physiological signal from the nervous system under standardized settings as a biomarker.” This biomarker is reflected back to the patient so they can change, he explains.
During a neurofeedback therapy session, the patient is coached to relax and focus themselves using various mental strategies; the practitioner is then able to objectively see if specific strategies are working, he notes.
All neurofeedback tools rely on a process called “operant conditioning,” says Dr. Colleen A. Hanlon, an adjunct professor at Wake Forest School of Medicine and the vice president of global medical affairs at BrainsWay. “This is a way of training the brain through carefully timed positive rewards,” she explains. “It’s the same principle parents use when teaching a small child to walk. Every time the child takes a step in the right direction, parents clap and cheer. That encouragement makes the child want to try again, repeating that healthy pattern, until walking smoothly becomes second nature.”
In neurofeedback, the “steps” are changes in brain activity. Sensors measure what the brain is doing, and whenever it moves in the desired direction, a positive reinforcement signal is given. That signal might be a movie playing smoothly, a game advancing, or even a virtual reality scene unfolding. Over time, this real-time feedback helps the brain practice healthier rhythms and patterns.
Neurofeedback—then known as electroencephalographic (EEG) biofeedback—was developed in the 1960s with early studies in epilepsy and ADHD, Hanlon explains. While the treatment progressed in the 1970s, it wasn’t until the 1990s that neurofeedback therapy was used regularly in clinical settings, following technological advancements and further research.

How does neurofeedback work?
A scientific principle called operant conditioning is the foundation of all neurofeedback techniques. You can think of it in terms of an aspiring athlete practicing free throws in basketball.
“Each time the ball swishes through the net, that satisfying sound and visual image is instant feedback,” Hanlon explains. “The brain locks in what worked, and over time the player refines their shot until it becomes automatic.” Neurofeedback therapy works the same way, she says, but instead of training your body to move in the correct pattern, you are training your brain to move in the right pattern, and taking advantage of the brain’s neuroplasticity.
Neurofeedback—a type of brainwave therapy—works through brainwave regulation, or the process of helping the brain balance rest and alertness, Hanlon explains.
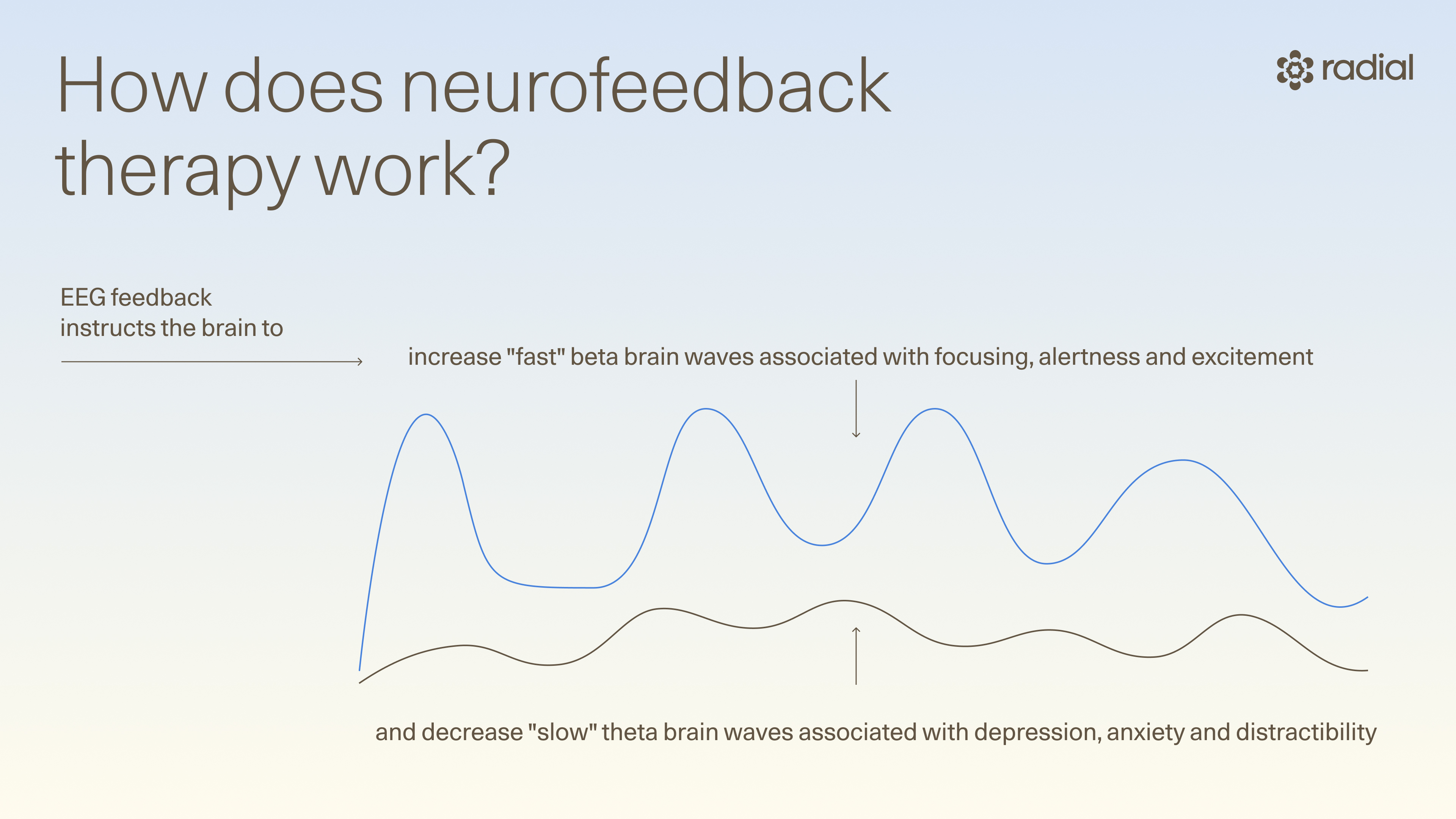
This is different from brain mapping therapy, which Tendler says is a marketing tool used by many clinics that produces a brief picture of the dominant frequency bands at a single point in time. Neurofeedback involves theta/beta training, which uses EEG feedback to instruct the brain to decrease "slow" theta brain waves associated with depression, anxiety and distractibility, and increase "fast" beta brain waves associated with focusing, alertness and excitement.
Types of neurofeedback
There are several different types of neurofeedback, including:
- Traditional EEG frequency training: Sensors placed on the scalp measure brainwave activity, which is then used to provide the patient with positive feedback, like visual or auditory cues, when desired brainwave patterns are achieved. Prism is an example of EEG frequency training.
- qEEG-guided brain mapping / LORETA: A process that records electrical activity across the scalp and compares it to large databases of normative brain activity, Hanlon explains. “This analysis highlights areas that are overactive, underactive, or not well synchronized with other regions,” she says. “Clinicians use this information to identify potential patterns associated with conditions such as ADHD, depression, or epilepsy, and to design personalized neurofeedback training protocols that target specific networks or regions of the brain. “ LORETA (Low-Resolution Electromagnetic Tomography) is a brain training technique that uses a computer to create 3D images of the brain and provides real-time feedback to train the brain's deep structures.
- Infra-low frequency (ILF): Focuses on extremely low frequency brain waves, typically below 0.1 Hertz.
- HEG (hemoencephalography): Uses infrared sensors placed on the forehead to measure brain blood flow and oxygenation levels.
What is Prism neurofeedback?
Prism is the first FDA-cleared self-neuromodulation software specifically designed for treating PTSD and depression. Like other forms of neurofeedback, it’s completely non-invasive and drug-free.
Prism self-neuromodulation uses reinforcement learning. “Individuals are using explicit trial-and-error attempts while looking at an interface that gives them feedback,” Tendler explains. “If they succeed, they are getting control over their mind.”
The treatment teaches you to control your brain using your own thoughts. A cap with EEG sensors measures your brain activity then turns them into a game-like experience where your personal experiences, emotions or memories control what happens on screen.
Prism is part of “the new generation of EEG-based, FDA-cleared systems [that] are practical, portable, and ready for broader clinical use,” Hanlon says.
What is neurofeedback used for?
Neurofeedback therapy is used to treat a variety of conditions related to mental and physical health. It was originally a neurological treatment. “It was used for helping patients regain speech, walking, and motor function after strokes,” Hanlon says. “But today psychiatry is one of the fastest-growing areas, with promising applications in PTSD, anxiety, depression, ADHD and addiction.”
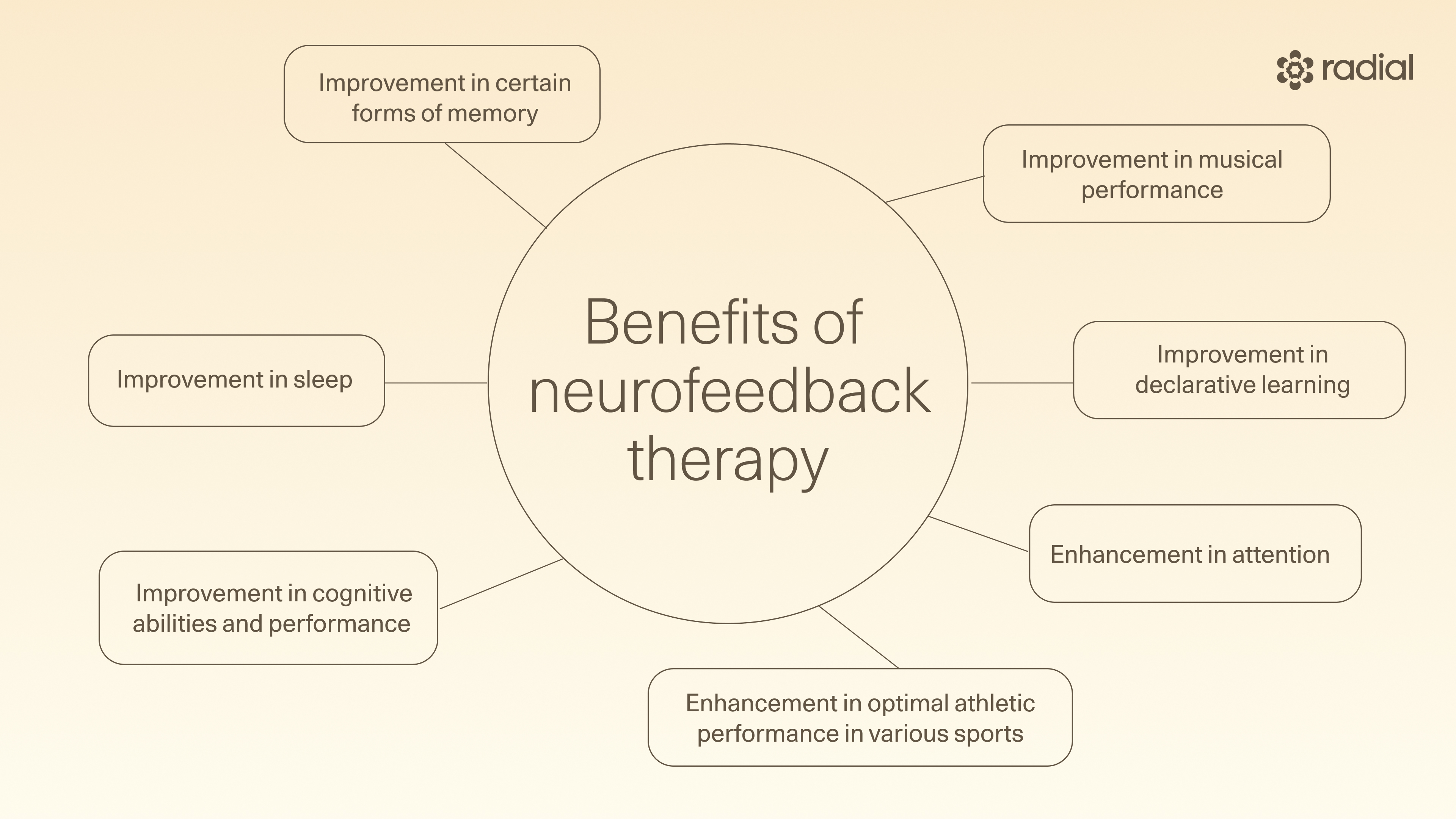
In addition to treating psychiatric conditions, there are a wide range of benefits of neurofeedback. For example, there is some research indicating that neurofeedback therapy may help enhance performance in healthy individuals, including:
- Improvement in cognitive abilities and performance
- Improvement in certain forms of memory
- Enhancement in attention
- Improvement in sleep
- Improvement in declarative learning
- Enhancement in optimal athletic performance in various sports
- Improvement in musical performance
Other neurofeedback benefits include the fact that the treatment is personalized and tailored to your specific symptoms, it gives you more control over your mental health, and with some types of neurofeedback, like Prism, no additional medication is required.
ADHD
There has been extensive interest in the use of neurofeedback to treat ADHD. Accumulated research led the American Academy of Pediatrics to recognize neurofeedback as a safe and effective treatment option for the condition in 2010.
Subsequent investigations have questioned that conclusion. For example, in a 2025 systematic review and meta analysis, researchers analyzed data from 38 randomized control trials with a total of 2,472 participants (ages 5 to 40 years) and found that “neurofeedback did not appear to meaningfully benefit individuals with ADHD, clinically or neuropsychologically, at the group level.”
There is also no evidence that neurofeedback therapy was more effective at treating ADHD than stimulant medications. The FDA has not approved neurofeedback therapy or cleared any neurofeedback devices as treatments for ADHD.
Depression
Neurofeedback therapy has shown positive results as a treatment for depression in a number of studies. While there is no single FDA-cleared neurofeedback device or treatment specifically for depression, some devices—like Prism—are cleared, based on accumulated evidence, to reduce symptoms of depression through promoting relaxation, reducing stress, and supporting general well-being.
PTSD
Life-threatening experiences have an immediate impact on how brain circuits communicate, and these neurological changes lead to lingering symptoms of PTSD, like reliving the experience or feeling jumpy and anxious. Medicine has little ability to effect these cell communication changes; at best, medicine decreases the intensity of the symptoms. But it does not address the underlying neurological changes that are producing the symptoms in the first place.
In addition to medication, typical PTSD treatment can include talk therapy and lifestyle changes. Talk therapy can help change our understanding of the trauma and can lessen symptoms. Lifestyle improvements can enhance resiliency and protect against the damage from living with a chronic stress response. Yet these modalities also address the symptoms of PTSD, without addressing the cause.
Neurofeedback is uniquely able to help the brain unlearn the patterns caused by the traumatic event and learn healthy ways of communicating again. Neurofeedback sessions are like exercise: repeat practice strengthens healthy patterns, eventually retraining the body’s response to triggers.
Research has indicated that quality neurofeedback therapy can treat PTSD effectively. By strengthening brain networks involved in stress and trauma processing, neurofeedback for PTSD reduces symptoms like hyperarousal, nightmares, and intrusive thoughts, and improves emotional regulation and coping skills. So far, there is only one neurofeedback modality FDA-cleared to treat PTSD: Prism.
Anxiety disorders
Neurofeedback for anxiety has shown promise as an effective treatment in a number of studies. For instance, a 2021 study found that neurofeedback can improve someone’s ability to practice mindfulness, which in turn, reduces anxiety. Additionally, neurofeedback may be an effective alternative to taking medication to treat anxiety disorders. The FDA has not approved neurofeedback therapy or cleared any neurofeedback devices as treatments for anxiety disorders.
Insomnia and sleep problems
The research into using neurofeedback as a treatment for insomnia and other sleep problems has been mixed. For example, a 2025 study found that alpha neurofeedback training mitigated insomnia with depression and anxiety. Additionally, a 2022 study concluded that neurofeedback is “a potentially powerful therapy” for a wide variety of neuropsychological disorders like insomnia. In a 2021 review, all 12 studies included showed that neurofeedback caused a clear improvement of subjective sleep. Meanwhile, other studies — like a 2024 systematic review and meta-analysis of randomized clinical trials and a 2017 double-blind placebo-controlled trial — found that neurofeedback didn’t improve sleep quality, or work any better than a placebo.
In 2024, the FDA cleared a neurofeedback device called the Modius Sleep for treating chronic insomnia.
Epilepsy
Neurofeedback has been used successfully in the past as an adjunctive therapy treating drug-resistant epilepsy. A 2022 systematic review found that neurofeedback therapy can be effective for seizure monitoring and management among those with epilepsy. Other research found that the treatment can help reduce seizure frequency. The FDA has not approved neurofeedback therapy or cleared any neurofeedback devices as treatments for epilepsy.
Other uses
In addition to the conditions above, neurofeedback has also been used to effectively decrease the symptoms of substance use disorders. However, a 2023 systematic review of the literature found that while there’s some evidence that real-time fMRI-based neurofeedback can restore brain function in people with substance use disorders, more rigorous experiments, including repeated measure designs with placebo control conditions, are required to confirm this.
While neurofeedback shows promise as a treatment for chronic pain’, a 2024 review of existing studies found that further research is needed to confirm this use of the therapy. Along the same lines, neurofeedback shows promise as a noninvasive and personalized treatment option for migraine. The therapy is also used to treat traumatic brain injury. According to a 2023 randomized control trial, low-resolution tomography Z-score neurofeedback resulted in improvements in memory, attention, and productive activity, while theta/beta neurofeedback improved memory and attention in patients.
Additionally, a 2018 study found that patients who appeared to respond to neurofeedback therapy for obsessive-compulsive disorder (OCD) or Tourette syndrome experienced continuing symptom improvement over the weeks following completion of the treatment. “It is possible that, having learned to control neural activity during neurofeedback, subjects continue to practice this newly acquired skill, which may result in continuing improvement of both symptoms and neural reorganization,” the authors of the study wrote.
There are also conditions where neurofeedback is marketed as an effective treatment, but the actual evidence is weak. “Some clinics market neurofeedback for things like ‘peak performance,’ dementia, schizophrenia, fibromyalgia, Lyme disease, or general ‘brain fog,’” Hanlon says. “These are intriguing areas, but the evidence is still early and not yet conclusive.”
What to expect in a neurofeedback session
Neurofeedback sessions are designed to be comfortable and low-stress. They typically take place in a dimly lit room with minimal distractions to help facilitate the neurofeedback training. After the person receiving neurofeedback therapy sits down, the neurofeedback therapist places sensors on their scalp to monitor brain activity.
“Patients then relax while watching a movie, playing a game, or engaging in a virtual reality scene,” Hanlon says. “When the brain moves in the desired direction, the feedback is positive. When it drifts, the feedback typically weakens or pauses. Over time, the brain figures out how to keep the feedback flowing, and those new patterns start to stick.”
After a neurofeedback session, people tend to feel relaxed yet alert, calm, focused, and able to solve problems. That said, people also experience some side effects following a neurofeedback session. These may include headaches, fatigue, irritability, or feeling spacey. Typically, these side effects resolve shortly after the session.
The treatment timeline and number of sessions varies depending on the type of neurofeedback therapy. “Think of it like practicing piano rather than taking a pill,” Hanlon says. Frequent sessions are required “spread over several weeks or months, to see meaningful results. This is similar to other noninvasive techniques such as transcranial magnetic stimulation (TMS).”
The Prism depression protocol involves 10 sessions lasting 30 minutes twice a week for up to eight weeks. The Prism PTSD protocol involves 15 sessions administered over 8 weeks, though some people may need longer treatments.
Neurofeedback safety, side effects, and risks
At this point, you may be wondering, “Is neurofeedback safe?” While generally safe and noninvasive, neurofeedback treatment side effects are possible.
Some of the most common include:
- Headaches
- Tiredness
- Mood swings
- Feeling high
- Nightmares
- Eye ache
- Confusion
- Nausea
However, the side effects don’t typically last a long time. “Side effects are usually mild and temporary,” Hanlon says. “They fade quickly, and compared with medication, the risks are very low.”
You may still have some questions, like “Is neurofeedback legit?” The short answer is that some neurofeedback modalities, like Prism, have received FDA clearance, and are therefore considered legitimate treatments for conditions like PTSD and depression. You may also be wondering, “Can neurofeedback damage your brain?” While certain types of neurofeedback lack substantial evidence of their effectiveness, the treatment is generally considered safe.
That said, just because neurofeedback therapy is widely considered safe, there are several red flags when it comes to getting the treatment. First, avoid getting the therapy from unlicensed clinicians or untrained practitioners. “It’s important to ask about training, certification, and clinical background,” Hanlon says. “Reputable providers will use standardized assessments, explain their methods clearly, use evidence-based tools, and adapt treatment as needed.”
One way to vet a neurofeedback therapist is to ask if they do quantitative EEG (qEEG) mapping and use that to guide protocols. If they don’t, opt for someone else. Additionally, stay away from any clinics or practitioners that make New Age-y claims about the treatment without providing data for review. Finally, don’t seek neurofeedback therapy at clinics that want to sell you large treatment packages—like 40 sessions—before they even assess your brain.
Cost, insurance, and at-home neurofeedback devices
Neurofeedback therapy costs vary depending on the provider, the location, the technology, and the type of treatment. According to Tendler, costs range from $250 to $500 for the hour.
Neurofeedback insurance coverage also varies, so it’s important to check with your insurer before making any treatment decisions. “Some plans cover it for ADHD or epilepsy, but many still consider it experimental,” Hanlon says.
According to Tendler, insurance coverage isn’t widely available yet, and occurs on a case-by-case basis. In a 2025 study, neurofeedback practitioners identified the high cost of the treatment and lack of insurance coverage as a major barrier to people accessing the therapy.
There are also ways to do neurofeedback therapy at home. It involves working with a neurofeedback device or neurofeedback machine outside of a clinic setting. “At-home devices can help with basic practice or mindfulness, but they’re not a substitute for professional care,” Hanlon says. “It’s like the difference between using a fitness app and working with a physical therapist. The app can be useful, but complex conditions usually need expert guidance.”
At-home neurofeedback training typically begins with using the device with an experienced practitioner in a clinic in order to get comfortable using it before bringing it home.
One major benefit of at-home neurofeedback therapy is that the treatment is more accessible to people who may not be able to make it into a clinic.
The future of neurofeedback
According to Tendler, neurofeedback therapy will continue to change the way certain mental health conditions are treated. “Practically, this is a paradigm shift in psychiatry, since it is teaching a skill rather than a passive treatment,” he says. This could have far-reaching implications. “In many ways, the future of neurofeedback isn’t just about rewiring the brain; it’s about retraining how we think about mental health itself,” Hanlon says.
Along the same lines, Hanlon thinks that we’ll see neurofeedback grow alongside other brain-based therapies, like transcranial magnetic stimulation (TMS). “TMS has already transformed the landscape for depression, OCD, and addiction,” she says. “Pairing that kind of external brain stimulation with neurofeedback’s internal self-training could create powerful new treatment pathways.”
Hanlon also believes that the next decade will bring more FDA-cleared technologies, like the recent approvals for Prism in PTSD and qEEG-guided systems for epilepsy. “These set the stage for broader adoption and insurance coverage,” she explains. At the same time, AI will likely help personalize training in real time, and portable devices will make therapy more engaging and widely available, she notes.
The bottom line
Neurofeedback therapy is a promising treatment for a variety of conditions including PTSD, depression, anxiety disorders, insomnia, and epilepsy. Because it’s drug-free and noninvasive, it is generally considered safe. Prism is the first FDA-cleared self-neuromodulation software specifically designed for treating PTSD and depression. With the right approach, symptoms of these conditions can ease and real relief is possible. Take the first step: reach out to Radial, we’ll help you open the door to healing.
Key takeaways
- Neurofeedback therapy is a non-invasive, drug-free type of biofeedback that measures brain activity in real-time, providing a feedback signal to help people train their brain to improve its function.
- Neurofeedback therapy has shown promise in treating conditions including PTSD, depression, anxiety disorders, insomnia, epilepsy, substance use disorders, OCD, Tourette syndrome, and traumatic brain injury.
- The most common side effects of neurofeedback therapy are headache and fatigue, and they typically go away shortly after treatment.
- The cost of neurofeedback therapy varies, but it can be quite expensive. At the moment, it is uncommon for insurers to cover the treatment.
Frequently asked questions (FAQs)
Is neurofeedback safe?
Neurofeedback is non-invasive, drug-free, and self-regulating—making it generally safe. It measures brain activity in real-time and provides a feedback signal to help people train their brain to improve its function.
How do you feel after a neurofeedback session?
After a neurofeedback session, people tend to feel relaxed yet alert, calm, focused, and
able to solve problems. That said, people also experience some side effects following a neurofeedback session. These may include headaches, fatigue, irritability, or feeling spacey. Typically, these side effects resolve shortly after the session.
Is neurofeedback safe for children?
Yes, neurofeedback therapy is generally considered safe for children. Neurofeedback is used as a noninvasive alternative for treating ADHD, PTSD and anxiety in children.
What are the benefits of neurofeedback?
Neurofeedback therapy is personalized and tailored to your specific symptoms, and gives you more control over your mental health. In addition to effectively treating a range of mental and physical health conditions, neurofeedback can also improve brain function, memory, attention and sleep quality.
Deep dive references
- Owen Muir, MD. PRISM: Trauma Treatment you Don’t Need to Talk About. Podcast. Released Aug 22, 2024. https://substack.com/@psychiatrist/p-147980013
- Phil Hulbig, Neurofeedback and Neuroplasticity. Podcast. Released Oct 10, 2025. https://philhulbig.substack.com/p/neurofeedback-and-neuroplasticity?utm_medium=reader2
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started



