Depression and ADHD: How to Tell the Difference and What to Do When It’s Both

Feeling down, unmotivated, foggy, and like your brain’s constantly on shuffle? Depression and ADHD might be teaming up—and figuring out which one is driving the bus is key to getting back on track. Let’s take a look at shared symptoms, key differences, and the best treatments for managing both.
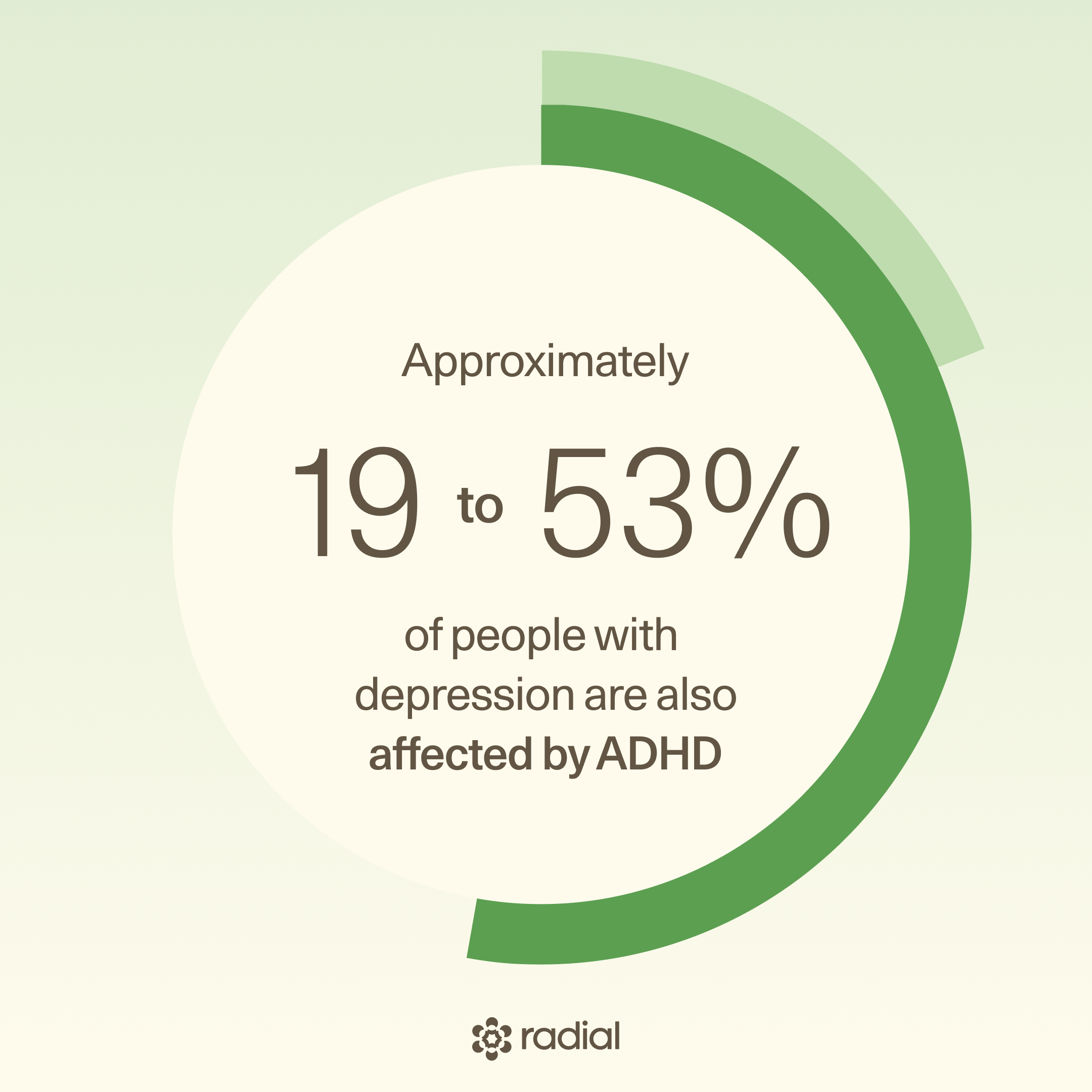
Depression and ADHD can feel like a double bind—you’re stuck in the fog of low mood and exhaustion, but your brain also won’t stop racing, distracting, or procrastinating. You’re not imagining it, and you’re definitely not alone. ADHD and depression in adults is common (some data estimates depression impacts up to 50% of people with ADHD), yet many don’t realize how closely the two are connected or how often one masks the other.
Just ask Stephanie Hartselle, MD, board-certified pediatric and adult psychiatrist and diplomate of the American Board of Psychiatry and Neurology. “I wasn’t diagnosed with ADHD until I was 36 and already a practicing doctor,” says Dr. Hartselle. “I’d had depression and anxiety, but once diagnosed, I realized ADHD was a major factor in those episodic disorders and receiving treatment has made an enormous difference in my life.”
Her story isn’t rare. Because ADHD symptoms can blur with or even contribute to depression, it’s common for people to spend years treating only part of the picture. The result? Ongoing frustration, burnout, and that nagging sense of why can’t I just get it together?
In this piece, we’ll break down how ADHD and depression overlap, how they differ, and what to do when you’re facing ADHD with depression—so you can finally get the right diagnosis, the right treatment, and gain a lot more self-compassion along the way.
What’s the link between ADHD and depression?
If you have ADHD and also struggle with low mood, you’re in good company. Roughly 70% of adults with ADHD have another mental health condition—most often depression or anxiety but also bipolar disorder, substance use disorder, or a personality disorder. Current data suggests depression may affect between 18.6% and 53.3% of those with ADHD.
In fact, research shows that adults with ADHD are three times more likely to develop major depression and six times more likely to have chronic low-grade depression (dysthymia) compared to those without ADHD. So, what’s behind this mind-muddling overlap? The connection runs deep—touching everything from genes to brain chemistry.
Genetics
ADHD and depression often run in the same families, hinting at a genetic link. Studies suggest that certain genes or genetic pathways may influence both conditions, increasing the odds of one showing up with the other. In other words, it’s not just bad luck—it’s biology.
Neurobiology
Brain scans show that both ADHD and depression involve differences in the frontal lobe, the region responsible for attention, emotional control, and decision-making. When this area doesn’t fire on all cylinders, it can lead to both distractibility and dips in mood. There can be gender differences on objective tests of cognition in ADHD, and and in depression, but their impact on cognitive tasks can overlap on some tasks and not on others.
Neurotransmitter issues
ADHD, dopamine, and depression–they’re all connected. Here’s how: Both conditions share similar neurotransmitter glitches—particularly abnormalities in dopamine and norepinephrine, two chemicals that help regulate focus, motivation, and mood.
Brain circuit dysfunction
There’s also a shared disruption in one of the brain’s emotion-regulation networks known as the LCSPT circuit (limbic-cortical-striatal-pallidal-thalamic). When this system falters, it can cause problems with reward processing—making it harder to feel pleasure or satisfaction, a key feature of both ADHD and depression. Already, specific brain circuit-based treatments modulating this circuit are beginning to show promise in depression research, and different circuit-based treatments are offering new hope in ADHD.
Impairment in executive function
People with ADHD and depression often share executive function challenges, like trouble focusing, organizing, or managing emotions. These cognitive hiccups can fuel rumination and rigidity—classic depressive thinking patterns. Struggling to regulate emotions or recover from setbacks can make someone with ADHD more vulnerable to developing depression over time.
Delayed brain maturation
The prefrontal cortex—home to impulse control and planning—may develop more slowly in people with ADHD. That lag may make teens and young adults especially susceptible to depression during key transition years when life demands more emotional and cognitive regulation.
While researchers are still untangling the full picture, one thing is clear: the ADHD–depression connection is real and complex. Understanding this overlap can help tailor treatments that address both conditions instead of tackling them in isolation (more on this later).
Can ADHD cause depression?
Let’s get this out of the way: ADHD doesn’t directly cause depression, but it can definitely set the stage for it. The connection is layered and complex, but if you’ve ever felt worn down by the daily grind of living with ADHD, it’s not hard to see how the two might coexist.
According to Dr. Hartselle, undiagnosed or untreated ADHD over time can raise your risk for depression. Why? Constant frustration, underperformance, and emotional rollercoasters can take a serious toll. When every day feels like a battle to stay focused or follow through, it’s easy to start feeling hopeless or defeated.
Part of the connection comes down to shared brain pathways and neurotransmitter glitches. People with ADHD often have lower dopamine activity, which affects reward and pleasure systems. That means it’s harder to feel joy or satisfaction (a concept known as low hedonic tone). Over time, that can snowball into symptoms like anhedonia (trouble feeling pleasure at all), along with sleep issues, irritability, and other depressive symptoms.
Then there’s the wear and tear that comes with living in a world that’s not designed for ADHD brains. Adults with ADHD often deal with challenges in executive function, memory, emotional regulation, and decision-making—all of which can ripple into work, relationships, and self-esteem. Over time, the stress of feeling misunderstood, underachieving, or constantly behind can fuel feelings of worthlessness or sadness.
The social impact of neurodivergence matters too. People with ADHD often struggle with interpersonal relationships, putting strain on friendships, romantic partnerships, and professional connections. Studies show that suicidal thoughts and behaviors are more common in people with ADHD than in those without (with suicide attempts up to four times more likely), especially when social struggles and social isolation go unaddressed.
Here’s the hopeful part: treating ADHD can reduce the risk of depression (and other comorbidities like anxiety, bipolar disorder, and substance misuse). Getting the right support—through therapy, medication, or both—can help you regain focus, manage emotions, and rebuild self-esteem before depression has a chance to take root.
ADHD vs. depression: Key differences and shared symptoms
ADHD and depression can look a lot alike—and that can make getting the right diagnosis tricky. Both can cause trouble focusing, low energy, and feelings of worthlessness. But understanding the differences (and where the two overlap) is key to finding the right treatment and support. Here’s what you need to know about ADHD and depression symptoms.
ADHD
ADHD isn’t one-size-fits-all—it actually comes in three main types:
- Predominantly Inattentive: You struggle to focus, follow instructions, or stay organized. Details slip through the cracks, especially with daily routines.
- Predominantly Hyperactive-Impulsive: You fidget, talk a lot, interrupt others, or act before thinking.
- Combined Type: You get a bit of both—distraction and impulsivity tag-teaming your brain.
But here’s the twist: ADHD often looks different in adults than in kids. Grown-ups may not be bouncing off walls, but they’re often battling mental restlessness, emotional ups and downs, and chronic exhaustion.
Common signs of adult ADHD include:
- Difficulty focusing or following through on tasks
- Disorganization and procrastination
- Forgetfulness and poor time management
- Restlessness or feeling “on edge”
- Impulsive speech or decision-making
- Trouble relaxing or winding down
- Emotional outbursts or low frustration tolerance
- Chronic fatigue and low motivation
Over time, these symptoms can mess with your confidence, relationships, and career—making ADHD a whole lot more than “just being distracted.” Adult ADHD often shows up as a chain reaction of real-world challenges, like:
- Relationship struggles: Studies show adults with ADHD are more likely to experience divorce and feel less satisfied in their personal, social, and professional lives.
- Academic roadblocks: In college, people with ADHD tend to have lower GPAs and graduation rates compared to peers without ADHD.
- Work and money woes: Time management, organization, and follow-through can be uphill battles. One study estimated that adults with ADHD earn $8,900 to $15,400 less per year than those without the condition, largely due to workplace challenges.
- Driving and safety risks: Impulsivity and inattention can spill over onto the road. Research found adults with ADHD are more likely to get traffic tickets, be in car accidents, and visit emergency rooms—one study showed 10 times more physician visits and triple the hospitalization rates compared to non-ADHD adults.
Depression
We all get the blues sometimes, but depression is deeper and more persistent. It’s a mood disorder that affects how you think, feel, and function day to day. Symptoms can range from subtle to severe, and no two people experience it exactly the same way.
Common signs include:
- Feeling sad, empty, or hopeless
- Losing interest in things you used to enjoy
- Big changes in appetite or weight
- Sleeping too little or too much
- Low energy or constant fatigue
- Restlessness or slowed movement/speech noticeable to others
- Feeling worthless, guilty, or like a burden
- Difficulty concentrating or making decisions
- Thoughts of death or suicide
It’s normal to feel down occasionally, but if these symptoms last most of the day, nearly every day, for two weeks or more, and start to impact your work, relationships, or hobbies, it could be depression.
ADHD and depression
Some people experience both ADHD and depression. As we know, depression can develop as a reaction to the daily challenges of living with untreated ADHD.
When it comes to diagnosis, “these two disorders have several overlapping symptoms,” says Dr. Hartselle—and that’s what makes telling apart ADHD paralysis vs. depression (or knowing whether someone’s dealing with both at the same time) so tough.
Shared symptoms can include, per Dr. Hartselle:
- Low self-esteem or self-worth
- Feeling incapable or unintelligent
- Poor memory or mental fog
- Executive dysfunction (difficulty planning, prioritizing, or managing impulses)
Other overlapping symptoms may include:
- Restlessness or psychomotor agitation
- Fatigue or low motivation
- Inattention
- Loss of pleasure or interest in activities (anhedonia)
In short, both can make your brain feel cluttered, your energy drained, and your confidence shot.

What happens when you have both ADHD and depression?
Real talk: having ADHD and depression can feel like a double whammy. Each condition is tough enough on its own. But together? They can amplify each other in ways that make everyday life feel like wading through quicksand. People living with ADHD and depression don’t necessarily have “hyperactive depression” but they do tend to face a heavier emotional and physical load: longer-lasting symptoms, reduced treatment response, and lower quality of life compared to those with just one condition.
So what does the ADHD-depression response feel like? Both conditions are linked to lower dopamine (the brain’s reward chemical) and lower norepinephrine (a neurotransmitter that affects mood regulation, attention, and arousal)—making it harder to feel pleasure, satisfaction, or motivation.
Then there’s the burnout factor. Constantly battling focus issues, emotional ups and downs, memory lapses, and decision fatigue can take a toll, especially when ADHD is left unchecked. Over time, that frustration and stress can snowball into depression (or anxiety).
ADHD often makes it harder to maintain friendships, navigate romantic relationships, or stay on good terms at work. That sense of disconnection can deepen depressive symptoms and even raise suicide risk. Research shows there’s a link between ADHD and suicidal thoughts: adults with ADHD are more likely to have suicidal thoughts or behaviors than those without, with lifetime rates of suicidal ideation reaching nearly 60%. Loneliness and social isolation—even in people without ADHD—can worsen suicide risk significantly.
Standout Box: If you’re feeling hopeless or thinking about harming yourself, please don’t go through it alone. Help is available. Call or text 988, or chat via 988lifeline.org to connect with someone right now.
Why misdiagnosis is common
Here’s the thing: ADHD doesn’t always look like bouncing off the walls. In fact, many adults with ADHD never got a diagnosis in childhood, especially if they weren’t the stereotypical “hyper” child, says Dr. Hartselle. That’s one big reason the condition often goes unrecognized, even though it affects an estimated 2% to 5% of adults worldwide.
People who didn’t have hyperactivity growing up—those quiet, compliant kids who weren’t disrupting class—often slip through the cracks. “Teachers are frequently dealing with overfilled classrooms and a quiet, compliant child who mostly completes work but is disengaged and uninterested can be missed for years,” says Dr. Hartselle. Over time, that same student may hear they’re “not working up to their potential,” struggle to keep up, or feel perpetually behind simply because they can’t stay focused, she says.
As frustration builds, self-esteem takes a hit, and anxiety or depression can creep in, says Dr. Hartselle. By adulthood, many of these people show up in a therapist’s office with those issues, not realizing ADHD is part of the picture.
Because clinicians are generally more familiar with mood, anxiety, or substance use disorders, they may treat depression or anxiety without ever addressing the ADHD. The result? Medications like SSRIs that don’t touch the core problem. Some estimates suggest that in the U.S., only about 11% of adults with ADHD are getting the treatment they actually need.
And then there’s gender bias. “Women especially can be missed for years,” says Dr. Hartselle. That’s because boys tend to show more outward, disruptive symptoms, while girls often internalize. Many bright, high-achieving women find ways to overcompensate for years, until one day their coping mechanisms just stop working, she says.
Add in another layer: people of color and LGBTQ+ individuals are also more likely to be overlooked or misdiagnosed due to systemic bias and limited representation in ADHD research, says Dr. Hartselle.
Bottom line? ADHD doesn’t always look how people expect it to, and that means far too many adults are still flying under the diagnosis radar.
How to tell if it’s ADHD, depression, or both
ADHD vs. depression: So, how do you know which one you’re dealing with when they share so many symptoms? The short answer: it’s complicated—but not impossible. With the right questions (and a little detective work), it is possible to tell whether you’re dealing with ADHD or depression (or to know you’re experiencing symptoms of both).
So, where do you begin? One key lies in when your symptoms start. “When we interview patients, first we try to get a sense of how long symptoms have been present,” says Dr. Hartselle. Depression tends to come in waves. “Patients can tell us when it started and what they were like before they felt depressed,” she says.
ADHD, on the other hand, usually isn’t new. “ADHD is a disorder that’s present from childhood,” explains Dr. Hartselle.
Clinicians often start with a few simple but telling questions:
- Have you had ongoing issues with attention and distractibility?
- Have these challenges stuck around for 10 or 20 years?
- If I saw you in the classroom as a kid, what would you have been like?
Family interviews or old report cards can also offer clues, says Dr. Hartselle. Not every kid with ADHD fits the “hyper” stereotype. In fact, teachers often describe the child—especially girls—as someone who “is quiet, follows directions, and gets fair to good grades,” Dr. Hartselle says. These subtle patterns can point toward ADHD that’s been missed for years.
To dig deeper, clinicians might ask, per Dr. Hartselle:
- Did you lose important things often as a kid?
- Needed instructions repeated?
- Feel like you had to work twice as hard as everyone else?
- Find sitting through boring tasks physically painful?
These questions alone can often reveal the diagnosis, says Dr. Hartselle.
If ADHD still seems likely, doctors may use screening tools to help confirm it. “We use scales for depression, anxiety, and adult ADHD,” Dr. Hartselle says.
Common diagnostic tools include:
Depression
- Patient Health Questionnaire-9 (PHQ-9)
- Beck Depression Inventory (BDI)
- Hamilton Rating Scale for Depression (HAM-D)
Anxiety
- Hamilton Rating Scale for Anxiety (HAM-A)
- Generalized Anxiety Disorder-7 (GAD-7)
- Yale-Brown Obsessive Compulsive Scale (Y-BOCS) for OCD
ADHD
- Adult ADHD Self-Report Scale (ASRS)
- Wender-Reimherr Adult Attention-Deficit Disorder Scale (WRAADDS)
- Conners Adult ADHD Rating Scales (CAARS)
- FAST MINDS (Forgetful; Achieving below potential; Stuck in a rut; Time challenged; Motivationally challenged; Impulsive; Novelty seeking; Distractible; Scattered)
While these scales can be helpful, Dr. Hartselle says the best way to confirm ADHD is still good old-fashioned conversation, plus collateral input from someone who knows you well, like a spouse or parent.
Note: Some clinicians may refer patients for neuropsychological testing, but that’s not always necessary. “ADHD is a clinical diagnosis,” says Dr. Hartselle. It’s “made by interviewing the patient” and collecting supporting evidence from others.
Neuropsychological (“neurospych”) testing can be useful for complex cases or learning differences, but it’s expensive (often $3,000–$9,000), not always covered by insurance, and can take months to schedule, she says. Most of the time, a well-trained primary care doctor or psychiatrist can make the diagnosis with the right background information.
What treatments are most effective?
Both ADHD and depression can be managed—and often significantly improved—with the right mix of treatments. From tried-and-true medications to newer, science-backed therapies, there are plenty of paths forward depending on your symptoms, needs, and comfort level.
For ADHD
Once ADHD is finally recognized (which can be half the battle), treatment can be highly effective, especially when it combines medication with lifestyle and behavioral strategies. Together, these can boost focus, emotional regulation, work performance, and even parenting skills.
Medication options
ADHD meds generally fall into two categories: stimulants and non-stimulants.
- Stimulants—like methylphenidate, mixed amphetamine salts, and lisdexamfetamine—are the traditional treatment options for ADHD.
- Non-stimulants, such as atomoxetine or alpha-2 adrenergic agonists, can also be effective, especially for those who can’t tolerate stimulants. Some antidepressants, like bupropion (an NDRI) and venlafaxine (an SNRI), may also help with ADHD symptoms. But it’s worth noting: selective serotonin reuptake inhibitors (SSRIs) (commonly used for anxiety and depression) don’t target ADHD directly and don’t typically relieve symptoms.
Non-medication approaches
Medication alone doesn’t always cut it, and that’s where non-pharmacologic strategies shine. Research shows that a multipronged approach—blending medication with therapy and skills coaching—leads to the best long-term outcomes.
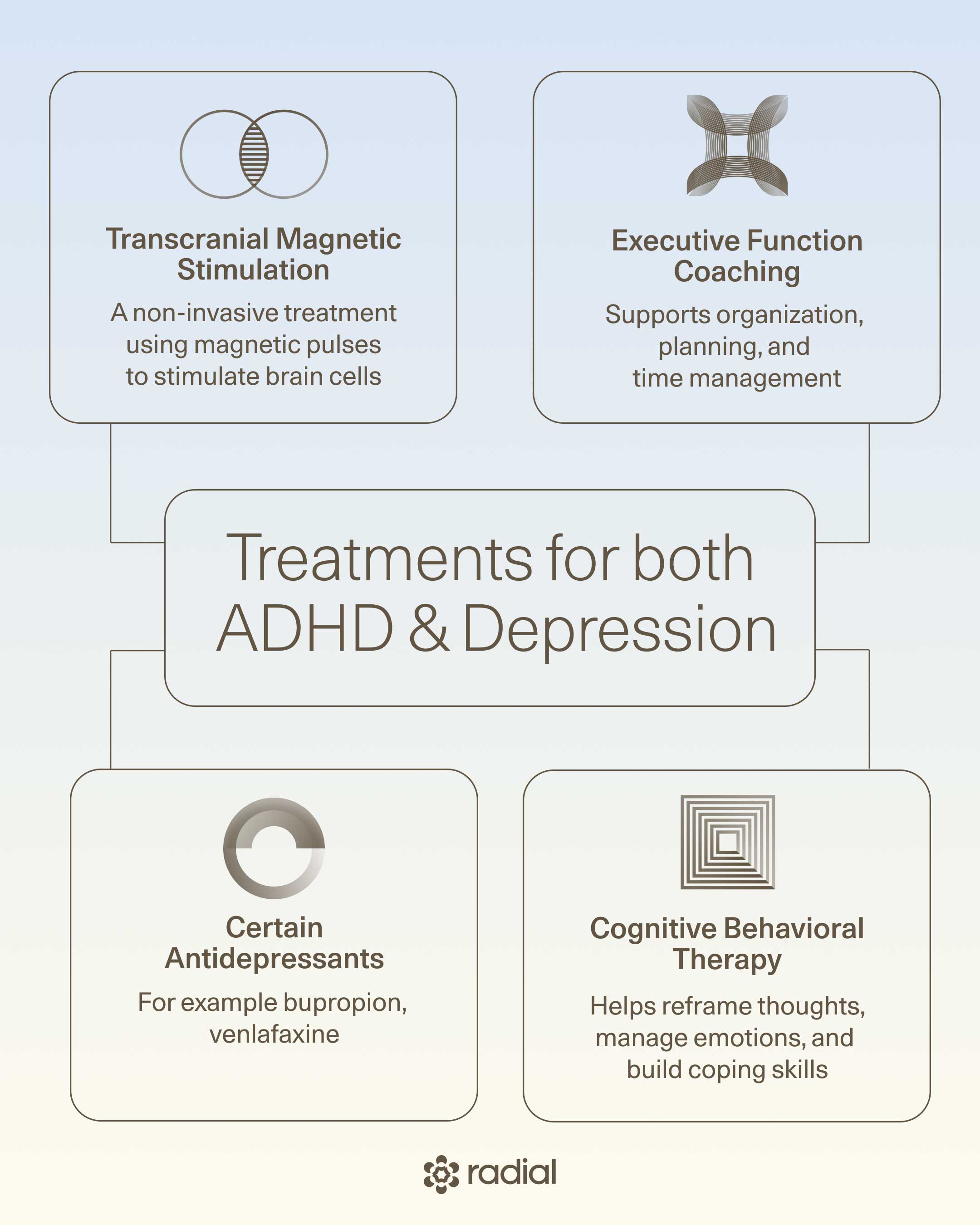
- Cognitive behavioral therapy (CBT): This form of therapy helps you challenge negative thought loops, build healthier habits, and regulate emotions. It’s particularly helpful for adults with ADHD who still struggle despite meds and can also reduce symptoms of depression and anxiety.
- Executive function coaching: Think of this as ADHD life training. Coaches help you master time management, planning, goal-setting, and organization. “It allows patients to feel more autonomous and efficacious in their lives,” says Dr. Hartselle.
- Monarch eTNS: This device-based treatment is FDA-cleared as a Breakthrough device in children, but not yet in adults.
Effectively managing ADHD can also reduce your risk of developing depression or anxiety down the road. Studies show that early ADHD treatment improves quality of life, lowers stress, and may even alter the trajectory of comorbid conditions over time.
For depression
Depression treatment is often a mix of therapy, medication, or both—but new, innovative options are emerging for people who haven’t found relief from traditional approaches.
Talk therapy
Talk therapy gives you space to unpack your thoughts, emotions, and behaviors with a trained professional. CBT, mentioned above, is also a very effective tool for managing depression.
That said, talk therapy alone doesn’t work for everyone. Only about one-third of people with major depressive disorder (MDD) reach remission with therapy alone, so it’s often combined with medication. Still, therapy remains invaluable, especially for processing emotions and maintaining progress once symptoms improve.
TMS therapy
If standard treatment hasn’t worked, transcranial magnetic stimulation (TMS) might. This non-invasive therapy—already FDA-cleared for major depression—uses magnetic pulses to stimulate specific brain areas involved in mood regulation, especially the dorsolateral prefrontal cortex (DLPFC), which is often dysregulated in depression.
Different types of TMS vary in stimulation depth, coil design, and session length, and your clinician can help determine which option fits best.
PRISM neurofeedback
Think of this as brain training meets video gaming. PRISM neurofeedback uses real-time neurofeedback—via a cap with electrodes—to help you retrain your brain’s reward and motivation systems. In one small study, 78% of participants saw improvement in depressive symptoms, especially anhedonia. Plus, this FDA-cleared therapy is non-invasive and has fewer side effects than many meds.
Ketamine therapy
Once known mostly as an anesthetic, ketamine has garnered evidence-based support as a viable therapy for treatment-resistant depression. It works differently from traditional antidepressants by restoring neural connections and improving communication between brain cells, often providing rapid relief.
Ketamine can be administered intravenously, intramuscularly, orally, or via a nasal spray (esketamine, an FDA-approved form called Spravato).
For ADHD and depression together
When ADHD and depression tag-team, treatment gets a little more nuanced. One approach is to start with whichever condition is most debilitating, then layer in treatment for the other.
- If depression hits hardest, focus on that first—treating it can improve motivation, concentration, and mood regulation.
- If ADHD is more disruptive, a long-acting stimulant can ease inattention and impulsivity, which in turn may lift mood and reduce frustration.
- If both are equally intense, they can be treated in close succession—but ideally not at the exact same time, so providers can track which treatment does what. Most providers start with depression.
A multimodal approach works best here too. Some effective strategies include:
- CBT: Helps reframe negative thoughts and process emotional challenges across both conditions.
- Executive function coaching: Builds structure, confidence, and a sense of self-efficacy, says Dr. Hartselle.
- Certain antidepressants: Bupropion and venlafaxine may help with both ADHD and depression. Bupropion “isn’t typically as effective as the stimulants, but if we are seeing both depression and ADHD, sometimes we’ll start with this antidepressant because of its different properties that affect dopamine release,” says Dr. Hartselle.
- Atomoxetine: A non-stimulant shown to improve ADHD symptoms and may reduce anxiety or depression.
- TMS: Early research suggests it may enhance ADHD outcomes in adolescents, especially for those who don’t respond to meds (between 10 and 30% of people treated for ADHD)—though more studies are needed.
- Avoiding ultra-processed foods: Studies show that eating a lot of ultra-processed foods—especially those with artificial sweeteners—may bump up the risk of depression. These sweeteners can trigger purinergic activity in the brain, which might play a role in mood disorders. There’s also evidence that diets high in sugar and saturated fat may worsen ADHD symptoms in kids.
- Exercise: Increasing data shows that physical activity can help dial down ADHD symptoms and boost executive function, likely because exercise increases neurotransmitters like dopamine, norepinephrine, epinephrine, and serotonin. Exercise is also a proven mood-lifter for depression—walking, jogging, yoga, and strength training all help by combining movement with social connection, mindfulness, confidence-building, nature exposure, and brain-based boosts in feel-good chemicals.
How to move forward
So you think it might be ADHD, depression, or both—now what? The next step is finding the right provider who can accurately diagnose and treat you. Sounds simple, but because ADHD is often missed or misdiagnosed, advocating for yourself can make all the difference.
Start by showing up prepared. “It’s best to come equipped with information the prescriber might need,” says Dr. Hartselle. Think of it like building your case—you’re giving your clinician the best possible evidence to work with.
Before your appointment, do a little “background check” with the people who’ve known you longest. Ask your parents or siblings questions like:
- Did I lose things a lot as a kid?
- Was my desk or room a constant mess?
- Did I seem zoned out or lost in thought a lot?
- Did you think I was living up to my potential at school?
- Does anyone else in the family have similar issues—or an ADHD diagnosis?
Then check in with your partner or close friend. Ask what they notice about your ability to complete projects, meet deadlines, or remember important things, says Dr. Hartselle. Do they see patterns of forgetfulness, lateness, or disorganization?
Encourage your clinician to speak with family members or your partner too—it helps them get a fuller, more accurate picture.
And don’t forget to bring “receipts.” That might include:
- Old report cards or teacher comments
- Performance reviews or work feedback about focus or follow-through
- Even your driving record—if you’ve had frequent accidents or insurance hikes, that could point to impulsivity or inattention patterns
Each of these details is like a puzzle piece that helps clarify what’s really going on.
Most importantly, if your provider isn’t taking your concerns seriously, don’t stop there. “If you’re experiencing depression, anxiety, or symptoms of ADHD and the provider isn’t listening, keep looking for someone who will,” says Dr. Hartselle. “Women, people of color, and LGBTQ individuals especially need to advocate more assertively, since symptoms in these groups are often overlooked.”
And if you’re feeling discouraged, that’s normal too. When you’re already battling ADHD and/or depression, finding motivation can feel like climbing uphill in molasses. But persistence matters. The right help is out there—you just have to keep pushing until you find it.
The bottom line
Above all else, remember: you are not broken. You’ve just been living in a world that doesn’t always support your needs. Depression and ADHD don’t define you, but understanding how they show up (and overlap) is the first step toward feeling better.
With the right provider, you can get clarity, real treatment, and a plan that fits your specific needs. Whether that’s medication, therapy, or newer options like TMS, there are tools that help you thrive, not just cope.
Ready to take that next step? Radial helps you access the latest fast-acting, evidence-based treatments. Connect with a licensed clinician virtually or in person who’ll listen, understand your story, and build a plan that finally works for you.
Key takeaways
- ADHD and depression can be present at the same time. Each can make the other worse, but getting the right diagnosis can help you finally connect the dots.
- Misdiagnosis is common. Especially in women, people of color, and LGBTQ+ folks—so self-advocacy matters.
- Treatment works. A mix of meds, therapy, and executive function coaching and lifestyle interventions can seriously boost mood, focus, and daily life.
- Alternative treatment approaches are available too. Innovative options like TMS and neurofeedback may help people who haven’t found relief from traditional therapies or who rather not take a pill.
- Addressing ADHD early can help prevent depression later. Managing one often lightens the load of the other.
- You’re not alone—and help is out there. Finding a provider who listens (and gets it) makes all the difference.
Frequently asked questions (FAQs)
Can I have ADHD and depression at the same time?
Yes—and it’s actually pretty common. Approximately 70% of adults with ADHD have another mental health condition (most often anxiety or depression). ADHD can make daily life feel chaotic and overwhelming, which can wear you down over time and trigger depression. On the flip side, depression can worsen ADHD symptoms like focus, motivation, and memory, creating a frustrating feedback loop.
Can ADHD medication help with depression?
Sometimes, yes. Though stimulant medications that treat ADHD are not designed to treat depression directly, they can boost energy, focus, and motivation—all of which can have a downstream effect and lift mood. One study even concluded that taking ADHD meds was linked to a lower risk of depression in the present and the future.
But if you’re dealing with both ADHD and depression, your provider might recommend combining ADHD meds with antidepressants or therapy for a more complete approach.
What is the best antidepressant for ADHD?
There’s no one-size-fits-all answer—it depends on your symptoms and how your brain responds. That said, some antidepressants (like bupropion) can help with both mood and focus. But not all antidepressants and ADHD work well together. SSRIs, for example, won’t do much to relieve ADHD symptoms.
Your provider can help find the right fit, whether that’s an antidepressant, ADHD medication, or a combo of both.
Why does ADHD cause depression?
While ADHD doesn’t directly cause depression, it can totally contribute to it. The link is layered and complex (scientists are still trying to figure it out), but here’s what we do know: undiagnosed or untreated ADHD over time can raise your risk for depression.
The simplest way to understand the connection between the two conditions is this: Living with untreated ADHD can be exhausting. Constantly feeling disorganized, misunderstood, or “lazy” can chip away at your self-esteem. Over time, that frustration and burnout can morph into depression, especially if your symptoms go unrecognized or unsupported.
Deep dive recommendations
- PJ Vogt. Why’d I take speed for 20 years? Part 1
- PJ Vogt. Why’d I take speed for 20 years? Part 2
- Huberman Lab. Episode 219. Improve Focus with Behavioral Tools & Medication for ADHD.
- Psychiatry and Psychotherapy Podcast. Episode 35. ADHD: Diagnosis, Symptoms & Treatment.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




