Teen Depression Treatment: Evidence-Based Options That Work
.jpg)
Teens with depression have to navigate the challenges of living with a mood disorder, along with the normal academic and social pressures of high school. A depression diagnosis may be unsettling, but there are several different ways to treat depression in teens — including some that are low-risk and highly effective. Being the parent or loved one of a teen with depression has its own challenges—help and resources are available for you, too.
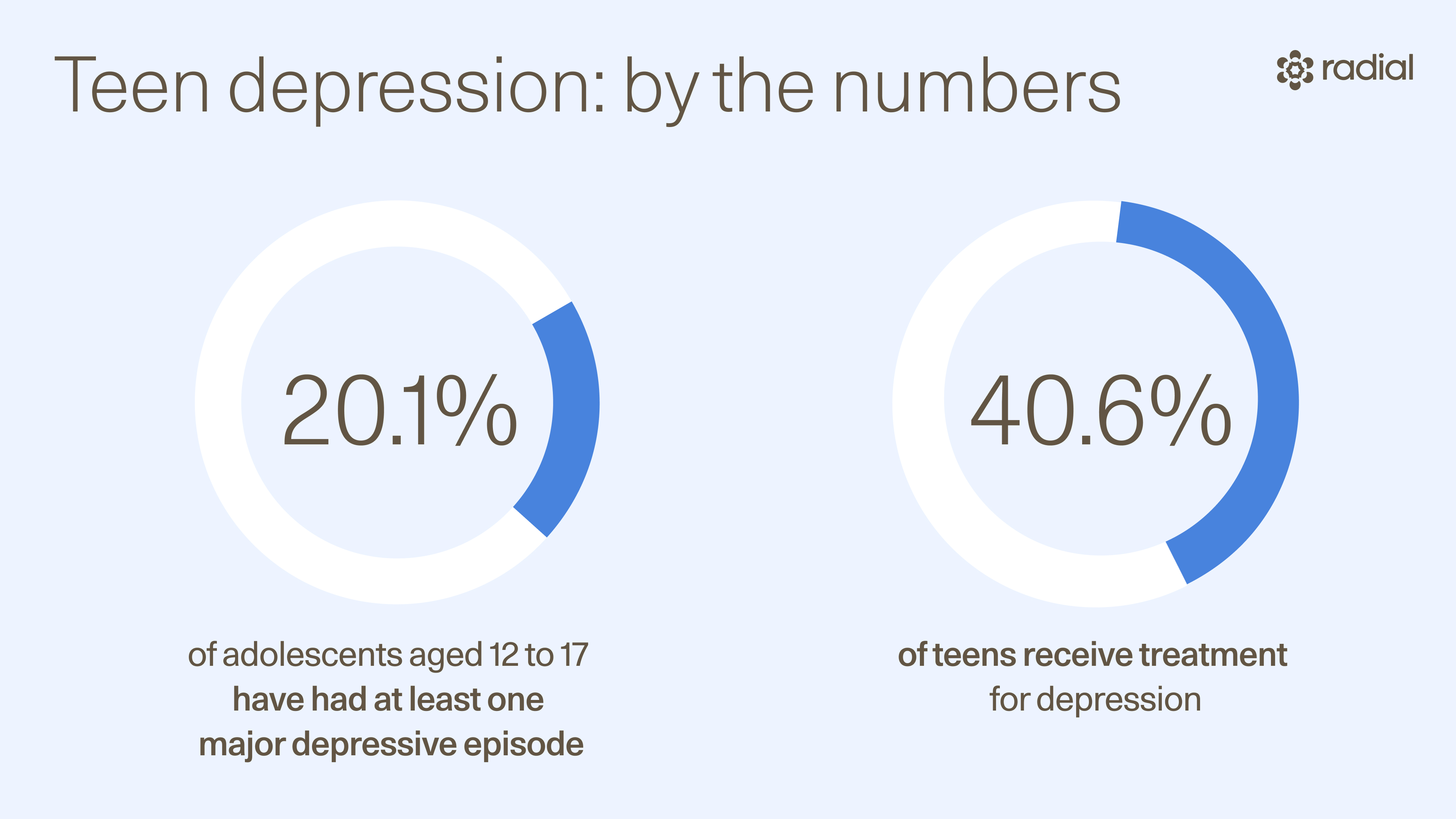
Depression can affect people of any age—including teens. In fact, the National Institute of Mental Health estimates that 5 million, or 20.1%, of adolescents aged 12 to 17 in the United States have had at least one major depressive episode. Yet despite depression in teenagers being quite prevalent, only 40.6% of teens with a major depressive episode receive treatment for the mental health condition.
Growing up, I was one of the depressed teens who didn’t get help. But it wasn’t for lack of trying.
When I was in high school, I’d periodically break down in front of my mother, telling her that I felt sad, empty, and hopeless all the time, and that nothing helped. I constantly felt guilty and worthless. To say I had low self-esteem was an understatement. Severe insomnia impacted my academic performance.
And yet, whenever I’d bring up going to therapy or talking to my doctor about how I was feeling, my mother quickly shut it down. She’d say things like, “Everyone feels sad sometimes—this will pass,” or “If someone finds out that you went to therapy, it could ruin your future career,” or “If people know you’re depressed, they’ll think I failed as a mother.”
This was the late 1990s, and the stigma surrounding teen depression and getting treatment for it was real. Instead of allowing teens to get the help they needed, parents like mine encouraged their children to “snap out of it,” “think positive thoughts,” or “pray about it.”
Things did change in my 20s, when I was out on my own and in control of my health-related decision-making. I started therapy and began to process what I was feeling and why, and learn about coping strategies.
Today, there’s no reason to wait that long, as both teens and their parents better understand the importance of getting help when it’s needed. If you’re looking for a clear, comprehensive, and compassionate guide to treatments for teen depression, you’ve come to the right place. We’ll talk about what works, what to expect, and how families can help.
What is teen depression?
Depression in teens is a serious mood disorder that causes ongoing feelings of sadness, emptiness, or hopelessness and a loss of interest in things someone used to enjoy. While it’s normal to be sad for a few days, depression can last for months or years.
Teen depression statistics vary, but globally, it’s estimated that 1.3% of adolescents aged 10–14 years, and 3.4% of 15–19-year-olds are currently experiencing a serious depression, according to the World Health Organization. “In any given year, a teen is more likely to have disabling depression than catching the flu,” says Eugene Grudnikoff, MD, a child and adolescent psychiatrist practicing in New York.
Symptoms of teen depression
Teens with depression have one or more of these symptoms most of the time:
- Sadness
- Feeling of emptiness
- Hopelessness
- Being angry, irritable, or frustrated, even at minor things
Other common symptoms of teen depression include:
- No longer caring about things you used to enjoy
- Changes in weight (e.g. losing weight when you are not trying to, or gaining weight from eating too much)
- Changes in sleep (e.g. having trouble falling asleep or staying asleep, or sleeping much more than usual)
- Feeling restless or having trouble sitting still
- Fatigue or not having energy
- Feeling worthless or very guilty
- Having trouble concentrating, remembering information, or making decisions
- Thinking about dying or suicide
“What distinguishes teen depression from normal adolescent angst and irritability is the disabling life effects,” Grudnikoff says. “Teens withdraw socially, struggle or give up academically. Some will try to self-medicate with marijuana or alcohol.”
Parents and family members play a crucial role in getting teens the help they need. “Some teens will go to some lengths to hide their depression or to power through it,” Grudnikoff says. “Many will feel better with time or with support from their family and friends.”
Signs of teen depression
They can start by recognizing the common signs of depression in teens. According to Johns Hopkins Medicine, these include:
- Feelings of sadness or hopelessness lasting more than two weeks
- Loss of interest in daily activities they previously enjoyed
- Loss of appetite, leading to weight loss, or increased appetite, leading to weight gain
- Difficulty falling or staying asleep, or an increased need for sleep
- Lack of focus and concentration
- Behavior changes at home or school (e.g., decline in academic performance, decrease in motivation, increase in arguments)
- General tiredness and low energy
- Irritability
It’s important for family members to be mindful of the signs of this mental health condition because severe depression in teens may lead to them considering or planning for suicide.
What to do if you think your teen is depressed
The first, most important step towards getting treatment is having your primary care doctor or a child psychiatrist do a professional assessment, like the PHQ-9 Modified for Teens. “Your child's pediatrician can be the first stop if you start having concerns about your teen’s mental health,” Grudnikoff says. “Other conditions such as anxiety, psychosis, trauma/PTSD, or OCD can mimic depression. Whatever the cause may be, seeing a pediatrician, a therapist, or a child psychiatrist will help with timely diagnosis and treatment.”
Evaluations will typically ask teens about things like:
- Their thoughts and feelings
- How they are doing at school
- Any changes in their eating, sleeping, or energy level
- Whether they are suicidal
- Whether they use alcohol or drugs
What's most concerning, however, is that teen depression can persist and become a life-threatening condition.
When to seek immediate help
If a teen with depression shows any indication that they are considering harming themselves or others, it’s time to seek help right away.
“Depression occasionally causes severe symptoms or life-threatening symptoms,” Grudnikoff says. “Severe symptoms can involve a teen who stops eating or spends hours in bed instead of going to school. Life-threatening symptoms include persistent hopelessness, self-injury, intrusive suicidal thoughts, escalating drug use, and suicidal behaviors.”
Concerned parents and family members should also pay attention to these warning signs of suicidal ideation and self-harm:
- Talking about or focusing on death or dying
- Talking of hopelessness or suicide
- Social isolation from friends or family
- Stopping activities that they previously enjoyed
- Giving away favorite possessions
- Increased risk-taking
- Engaging in self-harming behaviors
.jpg)
Suicidality and non-suicidal self-injury (NSSI)
Though we tend to lump suicide and self-harm together, there are key differences between suicidality and non-suicidal self-injury (NSSI).
Suicidality encompasses:
- Suicidal ideation
- Active suicidal ideation: someone has thoughts about taking actions to end their life, has a plan, and intends to act on it
- Passive suicidal ideation: someone might think about death or wanting to be dead, but has not made a plan and doesn’t intend to act
- Plans to die by suicide (i.e. having a specific method in mind to take one’s own life)
- Suicide attempts
- Suicidal behaviors
Motivation separates NSSI from suicidality. NSSI involves “repeatedly inflicting shallow, yet painful, injuries to the surface of the body with the intent to reduce negative emotions or to resolve an interpersonal difficulty, but with no intent to die,” the authors of a 2024 study published in the journal Children wrote.
NSSI behaviors may include:
- Cutting skin (especially one’s wrists or arms)
- Scratching skin
- Self-hitting or biting
- Banging one’s head against the wall
- Burning skin
- Picking scabs/interfering with wound healing
Most people who self-injure have tried multiple methods.
Crisis lines and emergency protocols
There are resources available for depressed teens experiencing suicidality or NSSI. It’s important to know that as isolating and lonely it can be to be a depressed teen or the family member of one can be, teen depression help is available. When immediate safety is a concern, there are resources available 24/7 - including crisis lines and emergency protocols.
Some of the national crisis lines include:
- Call (988), text (988), or chat
- Services for people who are Deaf and Hard of Hearing, including veterans
- A national network of more than 200 local crisis centers, combining local care and resources with national standards and best practices
- Text 741741
- Text, chat, or connect via WhatsApp
- 24/7 text-based mental health support and crisis intervention
- Call (1-866-488-7386), text (678678), or chat
- 24/7 counseling support for LGBTQ+ young people
There are also a number of local crisis lines, including those in Arizona, California, Delaware, and Texas.
Additionally, there are emergency protocols available from the American Foundation for Suicide Prevention.
How is teen depression treated?
There are a variety of treatments for teenage depression, including cognitive behavioral therapy (CBT), interpersonal therapy (ITP), mentalization-based therapy (MBT), family therapy, selective serotonin reuptake inhibitors (SSRIs), atypical antidepressants, transcranial magnetic stimulation (TMS), and SAINT TMS.
What therapies are effective for teen depression?
There are many types of talk therapy (psychotherapy) that can be part of a treatment plan for teenage depression. Therapy can be completed individually or as part of a group. Four types that have the best evidence of effectiveness are the following:
Cognitive behavioral therapy (CBT)
CBT is a form of talk therapy, and a first-line teenage depression treatment. It helps teens identify and change negative and unhelpful thoughts, and assists them in building coping skills and changing behavioral patterns.
The primary goal of CBT is to help people become aware of their automatic and negative thoughts and beliefs, as well as to challenge thought patterns in which they blame themselves for failures, but don't take credit for successes. CBT is a well-established depression intervention for adolescents, with multiple studies showing it to be effective. It is often used as part of combination therapy alongside antidepressants.
Interpersonal therapy (IPT)
IPT, a form of psychotherapy, focuses on improving relationships. It can help teens understand and work through troubled relationships that may contribute to their depression. IPT may help them change behaviors that are causing problems.
On top of discussing relationships, IPT also involves exploring major issues that may add to depression, like grief or life changes. IPT is also a well-established adolescent depression treatment, with multiple studies showing it to be effective.
Mentalization-based treatment (MBT)
Mentalization is the ability to understand one’s own thoughts and feelings, and the thoughts and feelings of other people. MBT involves someone focusing on how their present mental states affect their own behavior, which is particularly useful for teens with depression. The treatment may be especially effective in situations where a teen has “complex” depression—meaning depression co-occurring with broader personality and relational problems which are often related to a history of attachment trauma.
Family therapy
The goal of family therapy is to improve how a family functions as a unit, and as individual members. This can be especially helpful for teens with depression, as they often report problems in this area. Because depressive disorders may be the product of both genetics and environmental factors, some find therapy focused on improving family dynamics to be effective.
What medications are used to treat teen depression?
While depression medication for teens does exist, pharmacotherapy is not considered first-line unless the person’s depression is severe, or therapy is unavailable. Having said that, there are two categories of antidepressants for teens:
Selective serotonin reuptake inhibitors (SSRIs)
Selective serotonin reuptake inhibitors (SSRIs) are a type of antidepressant medications that work by increasing serotonin levels in the brain. The only two SSRIs that the Food and Drug Administration has approved for treating depression in teens are fluoxetine (Prozac) and escitalopram (Lexapro). They are considered the safest antidepressants for teenagers. These depression medications for teens should be prescribed alongside CBT: a combination which can result in greater symptom improvement.
It is important to mention that SSRIs carry a black-box warning from the FDA, the strongest type of the warnings that the agency can issue for prescription drugs. The FDA issued this warning back in 2004 highlighting that antidepressants increase the risk of suicidal thoughts and behaviors in children, teens, and young adults under 24.
The warning sounds both scary and counterintuitive; after all, how can medication help with suicidal thoughts (which are so common in depression), and cause them at the same time? The answer is based on the fact that every treatment has positive effects and side effects, which can have a degree of overlap. In the case of SSRIs, majority of teens will have positive effects, with fewer depressive symptoms and fewer suicidal thoughts; very few, perhaps 3 in 1,000, will experience increase in suicidality, a quite uncommon side effect.
It’s important to note that none of the children or teens in the clinical trials that led to the warning died by suicide, and that subsequent studies have called those early results into question. Nonetheless, pediatricians and psychiatrists use guidelines for best practices to prescribe SSRIs to youth safely with education and monitoring.
Other antidepressants
There are many non-SSRI antidepressants that can be prescribed for teenagers. These work by changing the levels of one or more neurotransmitters, like dopamine, serotonin or norepinephrine. While there is very little evidence that these atypical antidepressants help teens with depression, doctors may prescribe them if other medications have not worked.
What about Wellbutrin for teens? Also known as bupropion, Wellbutrin is another non-SSRI medication for depression that is often prescribed (but is not FDA-approved) for teenagers. Other examples of non-SSRI antidepressants include mirtazapine, nefazodone, trazodone, vilazodone, and vortioxetine.
What advanced treatments are effective for teen depression?
There are also two advanced, emerging, alternative treatments for depression in teens: transcranial magnetic stimulation (TMS) and SAINT TMS. These are among the newest depression interventions and are low risk and highly effective.
Transcranial magnetic stimulation (TMS)
TMS therapy uses magnetic fields to create small electric currents in the brain which target areas of the brain involved in depression, helping to adjust neural activity, improve mood over time, and assist in depression recovery. Unlike antidepressants, TMS does not increase the risk of suicidal ideation in teens, and therefore should be considered a first-line treatment.
SAINT TMS
SAINT is next generation TMS. Not only is it faster and more precise than traditional TMS and other depression treatments for teens, it also uses machine learning to personalize your treatment. Instead of several weeks, SAINT TMS takes five days to work.
What lifestyle changes and support strategies help teens with depression?
Other than various therapies and medication, you may be wondering how to help a teen with depression. Fortunately, there are other lifestyle changes and support strategies available. Lifestyle interventions that can treat depression include: optimizing restorative sleep, regular exercise/movement, diet changes (decreasing ultra high-processed foods), positive social engagement and avoiding toxins that can trigger/worsen depression (alcohol, cannabis).
When it comes to how to help teens with depression, don’t overlook sleep hygiene. “Having a consistent sleep schedule—yes, even on weekends—and getting at least eight to 10 hours of sleep each night is essential when it comes to combating symptoms of depression,” says Dr. Carlene MacMillan, dual board-certified adolescent psychiatrist and Chief Product Officer at Radial. This is especially important because when teens have delayed sleep phase syndrome, it often occurs alongside depression.
It may also help to request school accommodations for a teen with depression, like getting extra time on tests, a reduced courseload, and making up missed work. These may be formalized in a 504 plan: a legal document laying out the various strategies and accommodations in place to support a student with a disability. In this instance, depression can be considered a disability if the student’s depression substantially limits one or more of the student’s major life activities.
If you’re curious about how to help a teenager with anxiety and depression, then look into peer support. Just as a lack of social support can be a risk factor for depression in teens, adequate peer support can have the opposite effect. Peer support can happen formally, through organized support groups, or informally, through social interaction with friends and classmates.
Where can families find more tools and resources?
It’s important to remember that you’re not in this alone. Navigating depression in teens isn’t easy. For more information, check out the teen depression resources from these organizations:
- National Alliance on Mental Illness
- Mental Health America
- American Academy of Child & Adolescent Psychiatry
- Office of Population Affairs
- Los Angeles County Department of Health
- Society for Adolescent Health and Medicine
- Centers for Disease Control and Prevention
The bottom line
Teen depression is common and treatable. In fact, there are several different types of treatments for teen depression, including talk therapies, antidepressants, and neuromodulation. Keep in mind that families are not alone, and help is available. If you or a teen in your life is showing the signs of depression in young adults, it’s best to seek professional help and explore evidence-based treatments with trusted providers.
Key takeaways
- Depression in teens is a serious mood disorder that causes ongoing feelings of sadness, emptiness, or hopelessness and a loss of interest in things someone used to enjoy.
- The first, most important step towards getting treatment is having your primary care doctor or a child psychiatrist do a professional assessment.
- Treatments for depression in teens include therapy and antidepressants, as well as alternative depression treatment like neuromodulation.
- The only two SSRIs that the Food and Drug Administration has approved for treating depression in teens are fluoxetine (Prozac) and escitalopram (Lexapro).
- Lifestyle changes, like peer support, improved sleep hygiene, and school accommodations, may be helpful for teens with depression.
Frequently asked questions (FAQs)
Is teen depression a growing problem?
Over the past decade, rates of depression in teens have steadily increased. “The reasons for that are likely a combination of positive factors, like decreased stigma and increased screening and awareness, as well as more problematic factors, like excessive social media use and increased screen time at the expense of physical activity and unstructured free time in person with peers,” MacMillan says.
How many teens have depression?
The National Institute of Mental Health estimates that 5 million, or 20.1%, of adolescents aged 12 to 17 in the United States have had at least one major depressive episode.
What are the symptoms of teenage depression?
Teens with depression have one or more of these symptoms most of the time:
- Sadness
- Feeling of emptiness
- Hopelessness
- Being angry, irritable, or frustrated, even at minor things
Other common symptoms of teen depression include:
- No longer caring about things you used to enjoy
- Changes in weight (e.g. losing weight when you are not trying to, or gaining weight from eating too much)
- Changes in sleep (e.g. having trouble falling asleep or staying asleep, or sleeping much more than usual)
- Feeling restless or having trouble sitting still
- Fatigue or not having energy
- Feeling worthless or very guilty
- Having trouble concentrating, remembering information, or making decisions
- Thinking about dying or suicide
What are the coping mechanisms for depression in teens?
“Healthy coping mechanisms for teens can include finding creative outlets like art or music, having a trusted adult to confide in, and doing things that help others such as volunteering can all help lessen depressive symptoms,” MacMillan says. “In addition, structured evidence-based therapies for adolescents with depression, such as CBT and Dialectical Behavior Therapy (DBT), offer specific skills that can be extremely helpful.”
Deep dive resources
- Psychiatry and Psychotherapy Podcast. Episode 187: Best Diet for Mood Update 2023.
- Psychiatry and Psychotherapy Podcast. Episode 179: Exercise & Mental Health 2023 Update.
- Psychiatry and Psychotherapy Podcast. Episode 44: Marijuana and Mental Health.
- Rogers Behavioral Health. Parenting Teens with Depression Podcast.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started



