Ketamine Therapy Explained: Benefits, Risks, and What to Expect
.png)
Ketamine therapy is a fast-acting treatment option for depression, anxiety, PTSD, and other hard-to-treat mental health conditions. Ketamine can lift symptoms in hours, in contrast to the weeks or months it can take for traditional antidepressants to kick in. Here’s what it is, how it works, and what to know before deciding if it’s right for you.
If you’ve ever felt like you’ve tried everything for depression or anxiety—cycling through medications, switching therapists, doing all the “right” things—only to find yourself back in the same place, you’re not alone. That’s often where the conversation about ketamine treatments begins.
Originally developed as an anesthetic, ketamine has been repurposed in recent years as a treatment option for certain mental health conditions. Ketamine therapy benefits include its rapid onset and its potential to help when other treatments haven’t. In low, controlled doses, it can lift symptoms of depression, anxiety, PTSD, and chronic pain by acting on brain pathways that traditional antidepressants don’t target.
In this guide, we’ll walk through what ketamine therapy is, whether it’s right for you, and what to expect if you decide to try it.
What is ketamine therapy?
Ketamine was first developed in the 1960s as an anesthetic for surgery. But something surprising caught researchers’ attention: Some patients who’d been given ketamine for surgery or pain reported dissociation and euphoria. This wasn’t the intended effect, but it was consistent enough that scientists began to study why it happened.
Those studies led to a new use for ketamine: in low, carefully monitored doses, it can help relieve symptoms of certain mental health and pain conditions. Ketamine is prescribed for:
- Depression
- Suicidal ideation
- Bipolar depression
- Depression with obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Certain chronic pain conditions, like migraine and fibromyalgia
While the drug can alter mood and perception, ketamine is not an opioid, says Awais Aftab, MD, clinical assistant professor of psychiatry at Case Western Reserve University in Cleveland, Ohio. “Ketamine is a DEA Schedule III controlled substance, which is a substance classified by the government as having moderate abuse potential,” he says. “Due to this abuse potential, it is recommended that ketamine be administered under supervised settings.”
Indeed, research in people has linked frequent, unsupervised use to certain signs of addiction, like needing higher doses for the same effect, spending a lot of time seeking or using it, or continuing to use it despite harm. But controlled, low-dose ketamine given in a clinic for a set period of time shows a much lower risk of addiction. That distinction is important: When done safely, ketamine treatment is about healing, not harm.
The difference between ketamine and esketamine (Spravato)
You’ll hear both ketamine and esketamine mentioned in conversations about this type of treatment, and while they’re closely related, they’re not the same thing.
Ketamine is made up of two molecules, known as R- and S-ketamine. Esketamine therapy (brand name Spravato) contains only the S-ketamine molecule. That small chemical difference changes how the drug is processed in the body and how it’s regulated.
Here’s what ketamine vs. esketamine means in practice:
- Ketamine-assisted therapy for mental health is considered an “off-label” use, meaning the FDA hasn’t formally approved it for depression, anxiety, or PTSD (though it is approved as an anesthetic). It’s usually given by IV infusion or orally at specialized clinics, says Aftab. You’ll typically start with six to eight doses in the first few months, then maintain the effects with a maintenance dose every three weeks. Because it’s off-label, insurance rarely covers it, so most people have to pay out of pocket.
Esketamine is an FDA-approved nasal spray that can be prescribed for treatment-resistant depression and certain cases of major depressive disorder with suicidal thoughts. According to the prescribing information, you take it twice a week for the first month, once a week for the second, and every other week thereafter. Because it’s FDA-approved, it’s also more likely to be covered by insurance.

How does ketamine therapy work?
Scientists are still learning exactly why ketamine works for mental health, but we know it acts differently from most antidepressants. Instead of primarily affecting serotonin or dopamine, like common medications such as fluoxetine (Prozac) or bupropion (Wellbutrin), ketamine targets the brain’s glutamate system. This is the most common chemical messenger in your nervous system.
When given at a low, controlled dose, ketamine blocks the NMDA receptor in your brain. That sets off a chain reaction that can:
- Increase levels of brain-derived neurotrophic factor, a protein that helps brain cells grow and repair themselves
- Strengthen connections between brain cells, essentially “rewiring” areas that regulate mood and emotion
- Help the brain break out of rigid, negative thought patterns that fuel depression and anxiety
The result? For some people, mood lifts within hours—much faster than the weeks or months it can take for traditional antidepressants to kick in. That kind of relief can be life-changing, especially if you’ve felt stuck for a long time.
How ketamine is administered
There’s no single “right” way to receive ketamine therapy — your care team will guide you toward the option that’s safest and most effective for your needs. The method depends on your treatment goals, medical history, and whether you’re receiving ketamine or esketamine. Here are the options, according to Aftab:
- IV infusion: The most common off-label method, delivered slowly through a vein
- Lozenge or tablet: Dissolves under the tongue; sometimes prescribed for use between clinic visits
- Nasal spray: Includes the FDA-approved esketamine, as well as compounded ketamine sprays
- Intramuscular injection: A single shot into a muscle
Side effects and safety
It’s normal to feel a little nervous about what ketamine therapy might feel like in your body. The good news is that at the low doses used for mental health treatment, most side effects are mild and fade within a few hours. According to Dr. Aftab, the most common ones include:
- Dissociation
- Drowsiness
- Dizziness
- Nausea
- Headache
- Blurred vision
- Rise in blood pressure
- Sedation
There are also ketamine therapy risks to consider. Because the drug can briefly raise blood pressure and affect perception, you should consult with a cardiologist or neurologist if you have any underlying heart or brain conditions, says Aftab.
“For people with active psychosis or history of schizophrenia, ketamine could worsen symptoms,” he adds. “History of substance use problems also requires some caution.” That’s why treatments are always tailored and closely supervised—you can focus on healing while your providers focus on keeping you safe.
Ketamine therapy for mental health
Here’s a closer look at where ketamine-assisted therapy shows the most promise (and what the latest studies tell us).
Depression
Ketamine therapy for depression has the strongest track record—it can sometimes provide noticeable improvement within hours. So if depression has kept you feeling stuck, ketamine’s fast-acting effects may offer a breakthrough where other treatments haven’t.
According to Aftab, the types of depression that could benefit from ketamine include:
- Treatment-resistant depression (depression that hasn’t improved with standard medications or therapy)
- Major depressive disorder
- Depression with suicidal thoughts
- Bipolar depression
- Depression with OCD
- Severe depression without psychosis
While long-term research on ketamine for depression is still developing, the evidence so far is encouraging. A 2023 review of 14 studies found that combining esketamine with standard antidepressants can be an effective treatment for people with treatment-resistant depression.
Other research shows that IV ketamine infusions improve symptoms in major depressive disorder and bipolar depression, with benefits lasting up to a week after treatment. Importantly, esketamine is FDA-approved for major depressive disorder and for depressive episodes with suicidal thoughts, making it a structured and regulated option.
Anxiety
While research is still early, many people with anxiety are finding ketamine helps ease the constant cycle of fear and stress. Though researchers are still investigating how long the benefits last and whether maintenance sessions or combined therapies can make them more durable, early studies are promising.
For instance, one study found that people with anxiety who were given IV infusions of ketamine every 28 days had significantly less anxiety than those who did not.
PTSD
Living with PTSD can mean reliving trauma through intrusive memories, constant hypervigilance, or a body that never feels at ease. Ketamine may help by calming overactive fear pathways in the brain, making those symptoms feel less overwhelming.
Two clinical trials tested this directly. In one study, people with chronic PTSD who got a single IV ketamine infusion felt significantly better within 24 hours compared to those who got a placebo. Another study looked at repeated doses: People who had six ketamine infusions over two weeks showed clear improvements in PTSD symptoms, and for many, the relief lasted about a month.
While researchers are still learning how long the benefits last—and how ketamine might best work alongside established trauma therapies—these early results suggest it can offer a meaningful pause from the intensity of PTSD symptoms.
OCD
Obsessive-compulsive disorder (OCD) often traps people in rigid, repetitive thought patterns and behaviors that are hard to break. Early evidence suggests ketamine may help “loosen” these cycles, creating a bit of mental space where change feels possible.
In one small clinical trial, half of the participants who received just one dose of ketamine showed significant improvement in symptoms within a week, while none in the placebo group did.
According to Aftab, ketamine therapy may be most useful for people who have OCD alongside depression, but more research is needed before ketamine becomes a reliable option for OCD on its own.
Bipolar depression
Ketamine also shows promise for treating depressive episodes of bipolar disorder, says Aftab. Unlike some antidepressants, ketamine doesn’t typically trigger mania, making it a safer option when used carefully alongside mood stabilizers.
In two small clinical trials, patients with treatment-resistant bipolar depression received a single IV ketamine infusion while continuing their mood stabilizers. Compared to placebo, ketamine significantly reduced depressive symptoms within 40 minutes, and the improvement lasted for up to three days. A larger study showed similar rapid benefits when IV ketamine therapy was added to mood stabilizers.
These early results suggest ketamine can provide fast relief during depressive episodes, which can be a game-changer if you have bipolar depression. Because research is still ongoing, it’s considered an add-on treatment rather than a stand-alone option.
ADHD
Research on ketamine for attention-deficit/hyperactivity disorder (ADHD) is very limited. Some scientists are curious about whether ketamine’s ability to strengthen brain connections could support attention and focus, but the evidence isn’t there yet.
One recent computer-based study even explored a potential hybrid drug that combines ketamine with methylphenidate (a standard ADHD medication). The early findings suggested this combination could safely target depression and ADHD more effectively than either drug alone. But this was a lab simulation, not real-world research in people.
For now, ketamine isn’t a recommended treatment for ADHD, but it remains an area of curiosity as scientists search for new options to support people living with the condition.
Emerging uses
Beyond mental health, ketamine therapy is also being explored for other conditions. For instance, small studies suggest ketamine may help reduce cravings for people with alcohol, cocaine, and opioid use disorders. In one trial, people with severe alcohol use disorder who received ketamine infusion therapy had more alcohol-free days months later than those given a placebo.
Ketamine’s rapid antidepressant effects may also be valuable for people with late-stage terminal illnesses. Research shows it can quickly ease depression, and some patients also need fewer opioids. Similarly, ketamine shows promise in easing the chronic pain associated with disorders like fibromyalgia and migraine.
What’s more, early studies and case reports show ketamine may improve symptoms of anorexia and bulimia, sometimes leading to remission when paired with therapy.
Finally, pairing ketamine with therapy may help extend its benefits. Results so far are mixed, but studies in depression and substance use disorders suggest it may reduce relapse and cravings for some people.
Who is a good candidate for ketamine therapy?
Ketamine therapy isn’t right for everyone, but in the right situations, it can be a powerful tool. According to Aftab, you may be a good candidate if you have:
- Treatment-resistant depression
- Major depressive disorder
- Depression with suicidal thoughts
- Bipolar depression
- Depression with OCD
- Severe depression without psychosis
On the other hand, he says you may not be a good candidate if:
- You have active psychosis
- You have a history of schizophrenia
- You have a history of substance use disorder
- You have uncontrolled heart problems
- You’re pregnant or breastfeeding
- You’re a child
If you’re unsure whether you or a loved one might be a good fit, a Radial provider can help you sort through your options with compassion and care.
Ketamine therapy: what to expect
Trying something new for your mental health can feel daunting — especially if other treatments haven’t worked. Knowing what to expect before, during, and after a session can help you feel more comfortable and in control. Your care team’s job is to guide you through each step so you feel comfortable from beginning to end.
How to prepare for your first session
Before your first treatment, your provider will walk you through the process in detail and review your medical history. A few common steps include:
- Eating and drinking: Most clinics recommend avoiding food eight hours before an infusion, and fluids two hours before.
- Medications. Bring a list of everything you take, and your care team will let you know if anything needs to be paused or adjusted.
- Logistics: You won’t be able to drive afterward, so plan to have someone accompany you or arrange transportation home.
- Comfort: Some people bring headphones, an eye mask, or calming music for ketamine therapy.
What does ketamine therapy feel like?
Ketamine works differently than other antidepressants, and part of that difference is that you’ll actually feel it during treatment. Common sensations include:
- A sense of detachment from your body or surroundings (dissociation)
- Changes in how you perceive sound, light, or time
- Euphoria
- Pain relief
Some people describe ketamine therapy as calming or dreamlike; others find it disorienting at first. Either way, it’s normal to have mixed feelings, and your providers will be there to help you through it.
How many sessions are needed?
Ketamine therapy isn’t a one-time treatment. Most infusion protocols involve an initial series of three sessions over the course of a few weeks to first determine whether it has a beneficial effect. If it does, most people will go on to have an additional three to five sessions. Novel, flexibly-dosed, once-weekly protocols are being evaluated in cutting edge centers like Radial, which may improve the remission rates even further.
With esketamine, the typical schedule is more standardized: twice weekly for the first month, then once a week for another month, and then every other week as maintenance.
Ketamine vs. other treatments
Traditional antidepressants, psychotherapy, and brain-stimulation approaches like transcranial magnetic stimulation (TMS) remain first-line options for most people. Here’s how ketamine compares.
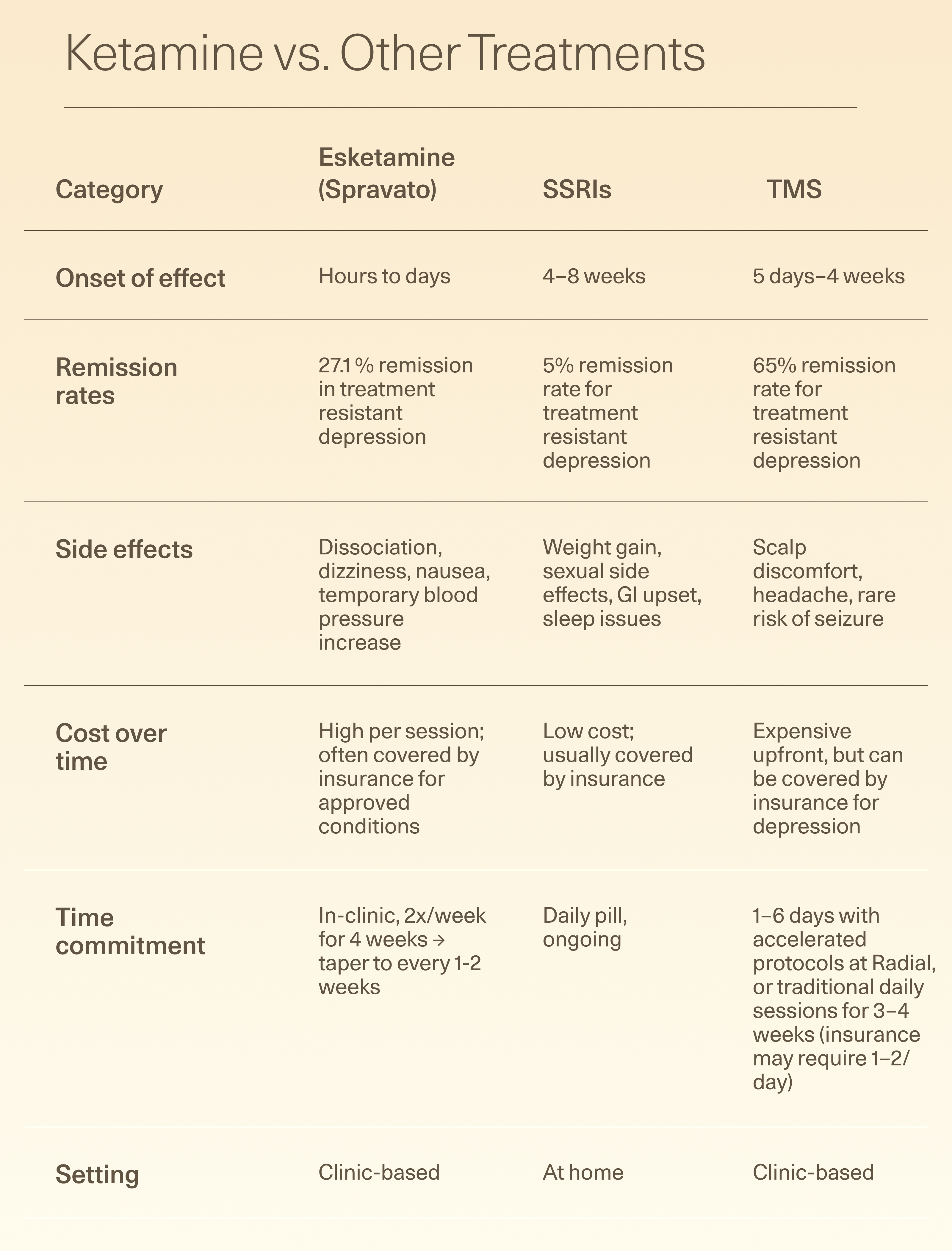
Traditional antidepressants, psychotherapy, and brain-stimulation approaches like transcranial magnetic stimulation (TMS) remain first-line options for most people. Here’s how ketamine compares.
Ketamine vs. SSRIs
Selective serotonin reuptake inhibitors (SSRIs) are one of the most commonly prescribed types of antidepressants. They’re effective for many people, but can take weeks to show results. Some people never respond at all.
Ketamine, in contrast, can begin to lift mood within hours. It also works through a different system in the brain, targeting glutamate rather than serotonin.
The trade-off is that SSRIs are inexpensive and widely available, while ketamine therapy requires in-clinic sessions, close monitoring, and often higher out-of-pocket costs. SSRIs can also be taken daily at home, whereas ketamine needs structured administration.
Ketamine vs. TMS
TMS is an FDA-cleared treatment option for people with depression who haven’t improved with medications, as well as conditions like OCD, migraines, and smoking cessation. It uses magnetic fields to stimulate brain activity. Like ketamine, TMS avoids the systemic side effects of oral medications and doesn’t require anesthesia
The time commitment depends on the protocol: Traditional TMS usually requires daily sessions (one or two per day) over three to four weeks, while accelerated protocols involve multiple sessions per day over one to 10 days. With Radial, some accelerated options take one day, five days, or six half days, depending on the device used.
Where ketamine has the edge is, again, speed: improvements can appear within the first session or two, whereas “traditional” TMS benefits may take weeks. Accelerated TMS, such as SAINT TMS, maybe work faster, but the ability to rapidly reduce suicidal ideation in some people as soon as the first dose is a common upside of IV ketamine treatment. On the other hand, TMS is non-invasive, doesn’t involve any medication, and doesn’t carry risks like dissociation or nausea. Both treatments are generally safe, and both are being studied for conditions beyond depression.
Ketamine vs. psychotherapy
Talk therapy is one of the most common mental health treatments. Ketamine isn’t meant to replace it, but in some cases the dissociative effects might help people engage more in therapy and prolong the beneficial effects. While early studies are promising, larger trials are needed before it becomes a standard approach.
Ketamine therapy cost and insurance coverage
So how much is ketamine therapy, and will insurance cover it? The answer depends on the type of treatment. Here’s the breakdown of the general costs:
- IV ketamine infusions: Infusion treatments can run $300 to $800 per session out of pocket. Because they aren’t FDA-approved for mental health, they’re rarely covered by insurance.
- Injections or lozenges: These treatments are typically cheaper than infusions, though they’re also not covered by insurance. Injections can cost you hundreds of dollars per dose, while oral medication can be similarly expensive–with no hope of insurance coverage.The FDA has issued specific warnings against these “compounded” ketamine products.
- Esketamine (Spravato): This nasal spray is FDA-approved for treatment-resistant depression and depression with suicidal thoughts, so it’s often covered by insurance with the right diagnosis. Without coverage, each 84-milligram dose can cost you around $1663.
The bottom line
Living with depression, anxiety, PTSD, or another hard-to-treat condition can feel exhausting, especially if you’ve already tried other options without relief. Ketamine therapy isn’t right for everyone, but for some, it offers a new path forward and a chance to feel better faster.
If you’re curious whether ketamine or esketamine could help, talking with a provider is the best next step. At Radial, our team is here to listen, answer your questions, and help you explore the treatment plan that’s right for you.
Key takeaways
- Research shows that ketamine therapy can lift symptoms of depression, anxiety, PTSD, and other hard-to-treat conditions within hours.
- Ketamine infusions, injections, and lozenges are off-label and usually self-pay, while esketamine (Spravato) is an FDA-approved nasal spray for treatment-resistant depression that’s more likely to be covered by insurance.
- Unlike common antidepressant medications, ketamine targets the glutamate system in the brain to help rewire mood pathways and break rigid thought patterns.
- Not everyone is a good candidate: people with active psychosis, schizophrenia, uncontrolled heart problems, or substance use issues should avoid ketamine therapy.
- Treatment requires an in-clinic commitment, and most protocols involve multiple sessions and ongoing maintenance rather than a one-time dose.
Frequently asked questions (FAQs)
Who is a good candidate for ketamine therapy?
Ketamine therapy may be a good option if you have treatment-resistant depression, major depressive disorder with suicidal thoughts, bipolar depression, or severe depression that hasn’t improved with other treatments. It may also help some people with anxiety, PTSD, or OCD. People with active psychosis, hypertension, uncontrolled heart problems, or a history of substance misuse are usually not good candidates.
Does ketamine therapy get you high?
Ketamine can cause feelings of dissociation, euphoria, or changes in perception during treatment, which some people might describe as feeling “high.” These effects are temporary and usually wear off within a couple of hours. In a clinical setting, the doses are carefully monitored for safety.
Is ketamine therapy covered by insurance?
It depends on the type of treatment. Esketamine (Spravato) is FDA-approved for treatment-resistant depression and is often covered by insurance with the right diagnosis. IV ketamine infusions and lozenges are considered off-label, so they’re usually paid out of pocket and can cost several hundred dollars per session.
Is ketamine therapy legal?
Yes. Ketamine is a Schedule III controlled substance, which means it’s legal when prescribed and administered by licensed providers.
Want to learn more? Take a deep dive:
Psychiatry and Psychotherapy Podcast. Episode 030: Ketamine and Psychedelics with Dr Michael Cummings. Released Sep 24, 2018
Psychiatry and Psychotherapy Podcast. Episode 137: Ketamine Update with Brandon Kitay, MD. Released Jan 27, 2022
Huberman Lab Podcast. Ketamine: Benefits and Risks for Depression, PTSD & Neuroplasticity. Released Aug 7, 2023.
The Frontier Psychiatrist Podcast, Ketamine in the Land of Taylor Swift. Released June 20th, 2025
The KevinMD Podcast. Ketamine, What PCPs Need to Know with Carlene MacMillan, M.D., FCTMSS, DFAACAP. Released November 30th, 2023.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started



