Is TMS safe? A Deep Dive Into Transcranial Magnetic Stimulation Side Effects
Transcranial magnetic stimulation (TMS) therapy is one of the most effective treatments out there for depression, OCD, and more. But just how safe is it? The short answer: it’s very safe with minimal side effects. Here’s everything you need to know about TMS side effects.
We’ve all seen those drug commercials that end with a rapid-fire list of side effects. And if a pill can have a long list of them, you may be wondering what transcranial magnetic stimulation (TMS) side effects are. Let’s just say a commercial for TMS would spend a lot less time on the subject.
“TMS is incredibly safe, much safer than any medications on the market,” says Aron Tendler, MD, a psychiatrist in West Palm Beach, Florida, “And the side effects of TMS are usually temporary.”
Still, TMS uses a device with an electromagnetic coil to influence brain activities, which can be intimidating for many patients, including Ari Trette. She felt some pre-treatment jitters before getting TMS for her depression and OCD. Today, people often ask her about transcranial magnetic stimulations side effects.
“Lots of people ask about pain during the treatment,” says Trette, “The initial feeling is hard to describe, as it is slightly painful but feels more like being poked. After a few minutes, you barely notice it and it just feels like tapping.”
What she couldn’t ignore, however, was how her life changed. “After TMS, I returned to my love of art, academics, and found a new passion for rock climbing,” says Trette, “I was able to fully immerse myself back in an academic college setting and take on a full course load. In addition, I returned to fostering my love for painting, sewing, drawing, and embroidery.”
Ahead, we’ll dive into common side effects of TMS, including how it changes patients’ lives for the better, and see how TMS stacks up against other treatments.
What is TMS, and is it safe?
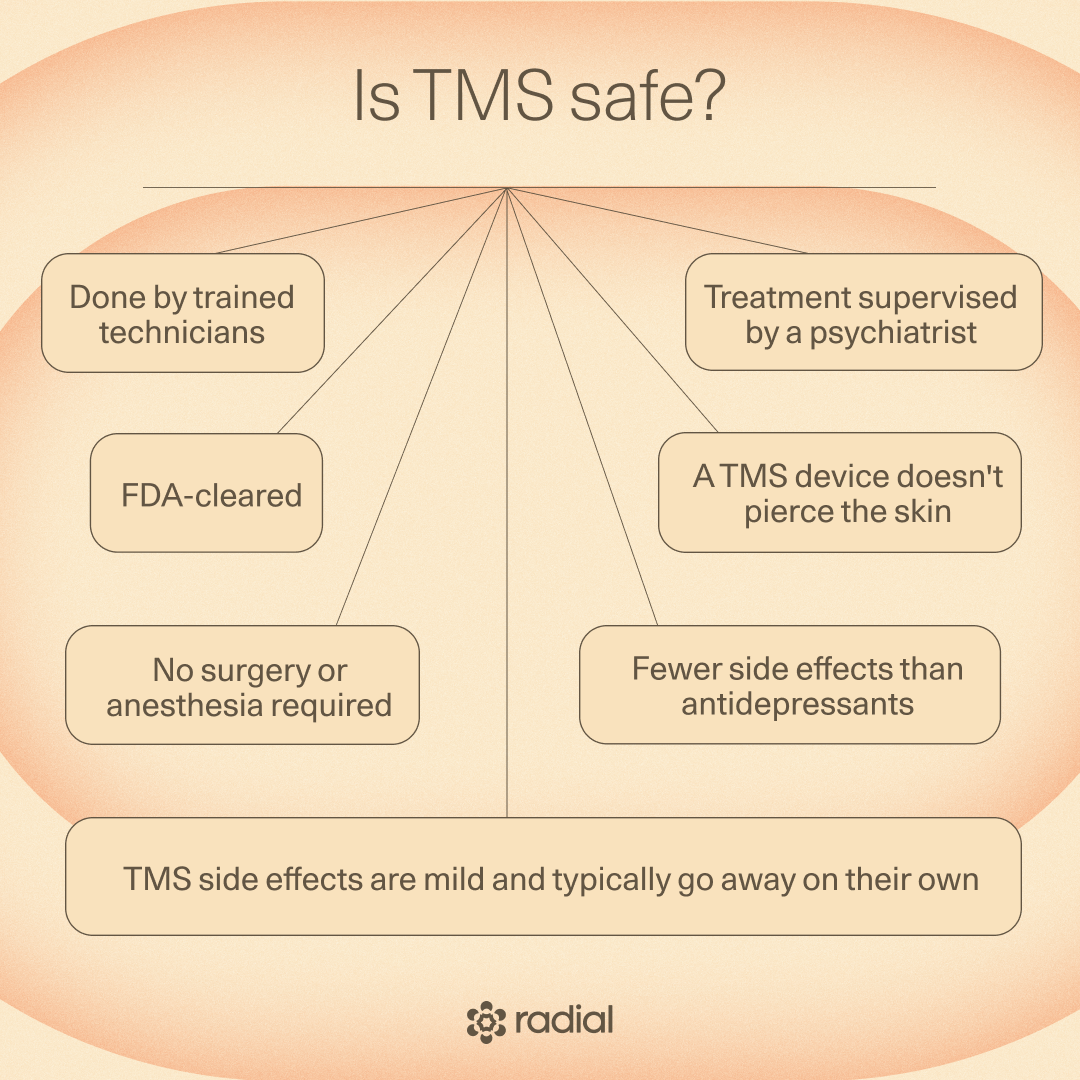
TMS therapy is a non-invasive, FDA-cleared treatment supported by extensive research. During a TMS session, a trained technician places an electromagnetic coil close to the scalp. The coil then delivers targeted magnetic pulses to specific parts of the brain. These pulses induce tiny electrical currents in the targeted regions, fine-tuning the activity of mood-related neurons.
That recalibration can effectively treat a range of conditions, and TMS is FDA-cleared for:
- Anxious depression
- Major depressive disorder (both in adults and adolescents)
- Migraines
- OCD
- Smoking cessation
It’s also safe for other uses that the FDA has yet to clear:
- Addiction
- Bipolar disorder
- Parkinson’s disease
- Postpartum depression
- PTSD
- Schizophrenia (specifically for auditory hallucinations)
- Stroke recovery
Admittedly, the idea of placing an electromagnetic coil near your head is a bit difficult to grasp, but the results speak for themselves: in one study, 81% of people with MDD improved after 30 sessions. Not only that, but TMS adverse effects are mild and usually temporary, and it has far fewer side effects than antidepressants. It’s also a noninvasive treatment. There is no surgery or anesthesia required, and the coil does not pierce the skin.
“For a treatment that can make such a meaningful difference in depression, OCD, anxiety, and more, it has an impressively light side-effect footprint,” says Colleen Hanlon, PhD, vice president of medical affairs at BrainsWay, “There’s no medication circulating through your body, no weight gain, no cognitive fog, no sedation—just focused magnetic pulses coaching specific brain circuits back into healthier patterns.”
What is a TMS session like?
During a TMS session, you sit in a chair with a cap or paddle with an electromagnetic coil resting close to your scalp. A TMS technician turns the device on, and it delivers electromagnetic pulses. In modern protocols, each session is short, lasting less than ten minutes.
A psychiatrist usually prescribes 25-50 sessions, depending on circumstances. For traditional TMS, someone completes one to two treatments each weekday for a few weeks until they’re done. While this approach works, results develop slowly.
But traditional TMS isn’t the only option. With some forms of accelerated TMS, someone can experience shifts in less than six days. Accelerated TMS is when someone undergoes five to ten sessions a day for one to six days in a row. For certain protocols, it not only leads to faster results, but has a higher efficacy rate, especially if someone gets Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT TMS). An early small trial at Stanford found that up to 90% of people with major depressive disorder go into remission with SAINT TMS compared to a smaller percentage with a course of traditional TMS.
Not every TMS center offers SAINT TMS. Magnus Medical has a search engine of centers who use this approach. You’ll find Radial centers in the search results, though you can always reach out to our team directly to learn more about this approach. SAINT isn’t the only form of accelerated TMS, and some insurances will cover accelerated protocols without neuronavigation.
What are possible TMS side effects?
Now that we’re all on the same page about what TMS is and just how well it works, let’s get into the side effects of TMS therapy. This won’t take long, since there aren’t many.
Common TMS side effects
“TMS is like a gym for your brain. There might be a little soreness at first, but with consistent sessions, people build improvements that last long after treatment ends,” says Dr. Hanlon, “Perhaps the biggest side effects are the positive gains in cognitive and physical health that come when the veil of depression is lifted from their shoulders.”
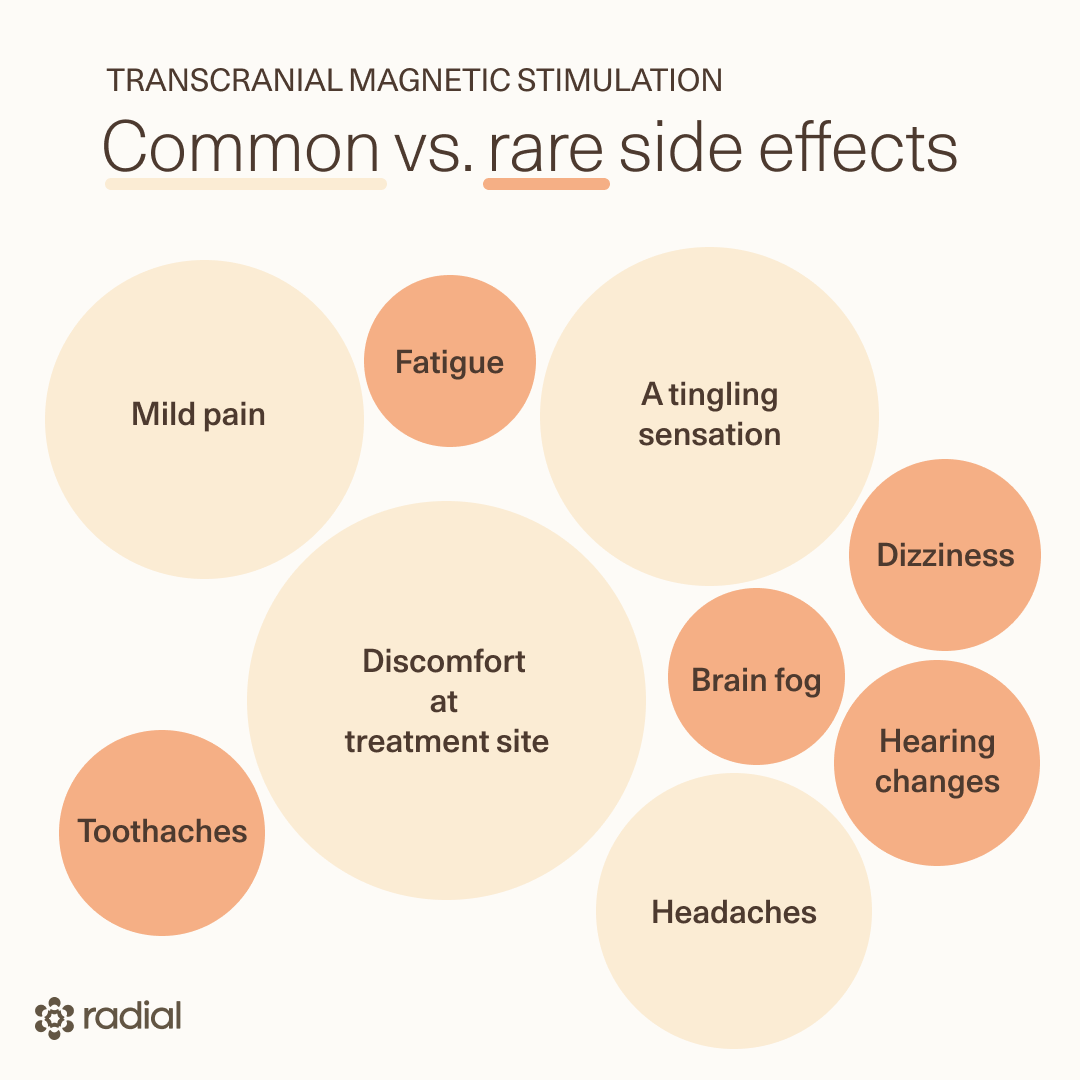
Besides this long term effect of TMS, there are a few other potential side effects. Typically, they’re not around for the long-haul and lessen as sessions continue. The most common are:
- Headaches: With about 35% of people experiencing headaches, this may be the most common adverse effect. As someone who gets migraines, the word headache scares me, but TMS headaches are not migraines. They are short, transitory headaches right after a TMS session. Typically, they go away on their own or with over-the-counter medications like Tylenol.
- Discomfort at treatment site: Almost 30% of people experience some discomfort at the treatment site during their treatment. This tends to be noticed more in earlier sessions, and it lessens or disappears as TMS sessions continue.
- A tingling sensation: Many patients report a tingling sensation on the scalp or head. Patients describe this as similar to being poked, and it goes away shortly after a session ends.
- Mild pain: Some people report pain in their neck, forehead, or jaw during treatment., This pain typically goes away on its own. An OTC pain medication may help.
Rare TMS side effects
The only thing rarer than severe adverse events from TMS are TMS long term side effects. In fact, most of the uncommon effects are temporary:
- Fatigue: Some patients feel more tired after a TMS session, which makes sense—TMS literally rewires neurons in your brain, which is hard work. TMS fatigue doesn’t last, and usually goes away on its own shortly after treatment
- Dizziness: Occasionally, someone may feel dizzy right after or during a session.
- Toothaches: Some people report a short-term ache in their teeth immediately after a TMS session. This often goes away on its own and occurs in less than 3% of people.
- Brain fog: Rarely, some people report feelings of TMS brain fog following TMS treatments. This is typically associated with fatigue and is temporary. In fact, some research suggests TMS may actually treat chronic brain fog or cognitive impairment.
- Hearing changes: During treatment, a TMS machine makes a loud clicking noise. Without proper protection such as simple earplugs, this can rarely lead to hearing loss or tinnitus. With proper hearing protection, the risk of hearing damage is very low, so skilled TMS technicians, like the team at Radial, will have something on hand to protect your ears. There are TMS protocols that may even treat chronic tinnitus, though researchers are still looking into this.
One of TMS’ most serious side effects is also one of its rarest: seizures. Fewer than 1 out of 1,000 patients experience it, which is less than 0.1%. “One of the biggest misconceptions is that TMS is the kind of treatment that causes seizures,” says Dr. Hanlon. “The seizure risk with TMS is extremely low— lower than the risk associated with antidepressants like SSRIs and SNRIs, and lower than the risk with medications like bupropion,” she continues, “It’s also significantly lower than the seizure risk from situations such as extended sleep deprivation or alcohol withdrawal.” And in the unlikely event that TMS results in a seizure, it'll happen right there during the treatment in the safety of the office.
One thing we know for sure is that there is no evidence of TMS memory loss or TMS brain damage. Not only are these myths, but TMS is known to boost the brain's own ability to grow new dendrites and connections. This might be why early evidence suggests that TMS enhances memory.
How TMS side effects compare to other treatments
If treatments for depression and other mental health conditions received report cards, TMS would receive a great score in safety (and probably effectiveness, too). Just look at how it compares to three other popular treatments:
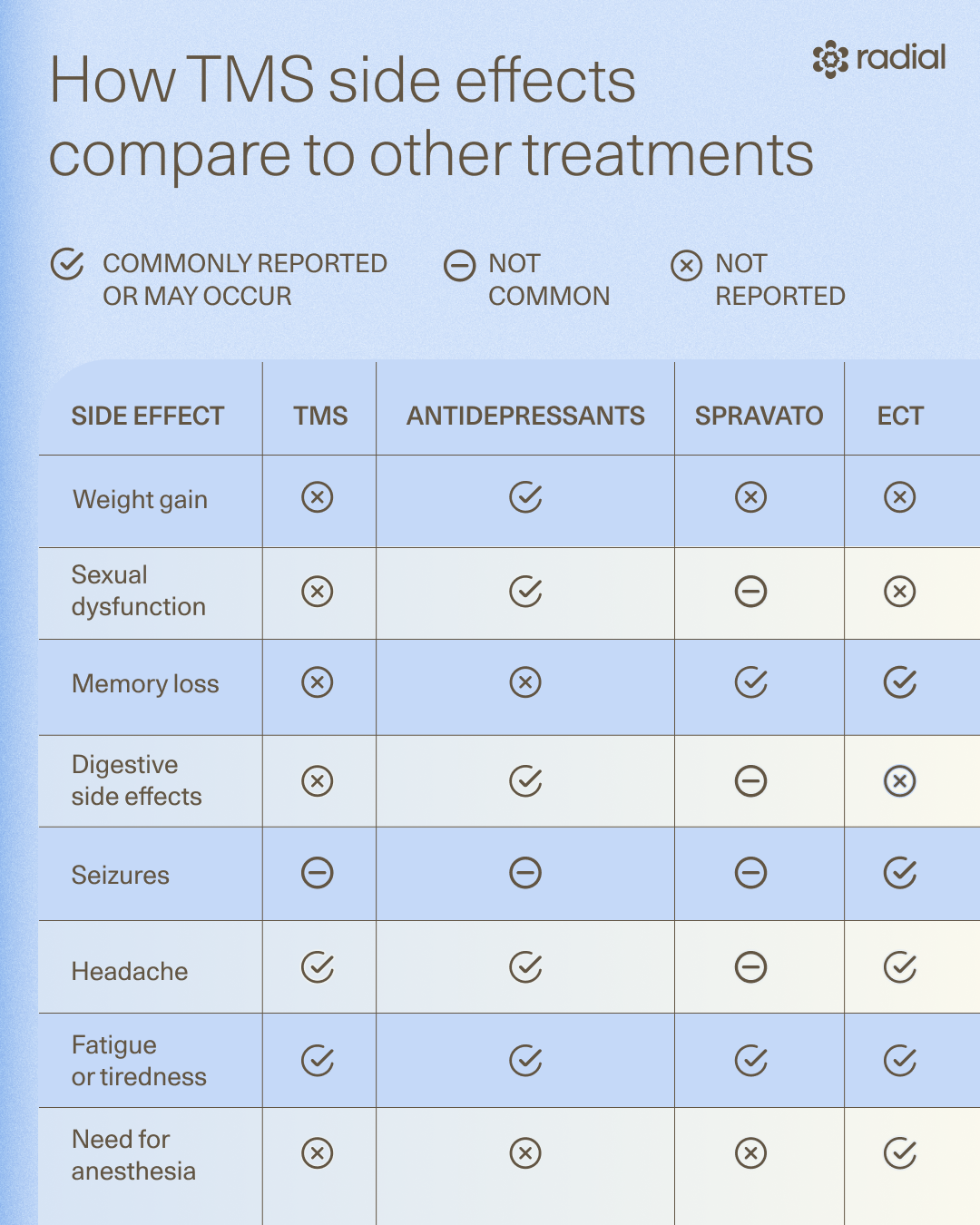
TMS side effects vs. antidepressants
Antidepressants refer to a few medication classes that block reuptake pumps responsible for clearing mood-regulating neurotransmitters. In turn, this improves the way the brain regulates mood, although the full effects take weeks to show up. The most commonly prescribed antidepressants are selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs).
While prescribed often, these medications come with a laundry list of potential side effects. A 2020 study polled 508 people on antidepressants and found the most common side effects were:
- Abdominal pain
- Nausea
- Diarrhea
- Constipation
- Sweating
- Weight gain or loss
- Swelling
- Dry mouth
- Headaches
- Lower libido
- Sudden heat stroke
- Sleeping too much or too little
In fact, antidepressant side effects are a primary motivator for people to explore TMS. In a 2025 study, researchers interviewed patients on what they liked about TMS, and they overwhelmingly mentioned how few side effects TMS had compared to antidepressants. Psychiatrists also refer patients to TMS when antidepressants don’t work because TMS can be more effective.
The study’s participants pointed out another big TMS benefit: it’s not a medication that has to be taken for a long time. One interviewee reflected, “Being at a fairly young age, I did not want to start a conventional treatment, a medication that would require to be continued for many years. I wanted something that can be applied in the short term.”
TMS vs. ECT
Like TMS, electroconvulsive therapy (ECT) is a brain stimulation therapy with a high success rate; one study suggests it has a response rate of 73%. Yet the two have some fundamental differences, including their safety profiles.
While TMS is non-invasive with few side effects, ECT is considered invasive since it requires anesthesia and induces a seizure (with ECT, a seizure is required for it to be effective).
ECT side effects include:
- Headaches, which only last a short while after an ECT session
- Confusion or fatigue, which is usually temporary
- Changes in blood pressure
- Memory loss
- Muscle soreness
- Rapid heart beat and a higher risk for other heart problems
TMS vs. Spravato
Spravato is a newer medication that may significantly reduce depression. It has been FDA-approved for treatment resistant depression and depression with acute suicidality since 2019 and produces a similar effect to antidepressants, though it works faster and comes with fewer side effects.
Most side effects of Spravato are limited to a couple of hours after each Spravato treatment session. Those potential side effects include:
- Sleepiness or fatigue
- Dizziness
- Feeling disconnected from yourself or your thoughts
- Changes in breathing while on medication
While Spravato is a game-changing medication for depression, it does have more side effects than TMS and may be more difficult for some people to tolerate.
The FDA label notes that Spravato’s most frequent side effects include dissociation, dizziness, nausea, vomiting, sedation, blood pressure increases, anxiety, and altered taste, along with urinary symptoms such as urinary urgency, frequency, dysuria, and cystitis-like discomfort. Most effects peak within the first hour after dosing and improve before discharge from the clinic.
Digestive side effects like nausea and vomiting are among the most frequently reported reactions with Spravato. In clinical trials, nausea occurred in roughly 25–30 percent of patients, and vomiting in 8–10 percent, usually within the first two hours after dosing.
Dissociation is the most characteristic side effect of Spravato. Patients may experience changes in perception, time, or surroundings, or feel detached from themselves. These effects peak about 40 minutes after dosing and typically resolve by the end of the required monitoring period.
Spravato can cause short-term increases in blood pressure, which is why blood pressure is checked before and after treatment and patients are monitored for at least two hours. These elevations usually peak around 40 minutes after dosing and return toward baseline by 1.5–2 hours.
How to minimize TMS treatment side effects
TMS side effects are already minimal, though there are some ways to make sessions more comfortable and successful. “In the first few sessions, [some patients prefer to] premedicate with either ibuprofen or acetaminophen,” recommends Dr. Tendler, “This will reduce the pain and the expectation of pain, which in its own right makes the pain worse.”
Dr. Hanlon adds that minimizing TMS side effects is a bit like settling into a gym routine. At first muscles ache, but you feel physically healthier with time. “In the first few sessions you might feel mild scalp discomfort or a light headache. These sensations usually fade quickly as your brain adjusts to the routine,” says Dr. Hanlon, “Then, just like the real gym, the magic isn’t in the first workout, it’s in the consistency. People start noticing deeper sleep, steadier energy, clearer thinking, and a gradual lifting of symptoms.”
You’re also not alone during treatment or when managing any side effects. TMS is done by trained technicians under the guidance of a psychiatrist. Your team will work with you to make sure sessions are as comfortable as possible before, during, and after sessions.
Who should (and shouldn’t) get TMS
Because there are so few TMS risks, it’s a pretty safe treatment for most people. It’s a particularly attractive option for those who may need to avoid antidepressants, such as those who are pregnant or postpartum, those with cardiac or renal dysfunction, and anyone who suffers severe effects from antidepressants.
That said, it isn't right for everyone. TMS contraindications are split into absolute (meaning you definitely can’t do TMS) and relative (which means if can be considered with careful evaluation, risk-benefit discussion, and protocol adjustment).
The only absolute contraindications to TMS are ferromagnetic or electronic implants in or near the head that could move, heat, or malfunction in a magnetic field, such as cochlear implants, aneurysm clips, deep brain stimulators, or metal plates close to the coil.
Other factors — including a history of epilepsy or seizures, traumatic brain injury, implanted cardiac devices, or medications that lower seizure threshold — are considered relative contraindications,
The bottom line
While TMS’ uniqueness causes some to hesitate, it’s a safe, FDA-cleared, non-invasive option. Its effectiveness and minimal side effects speak for themselves, especially compared to other options like antidepressants or ECT. If interested in learning more about TMS, reach out to Radial. We’ll help you find the evidence-backed treatment that works for you.
Key takeaways
- TMS is an effective treatment for anxious depression, major depressive disorder, migraines, OCD, smoking cessation, and more. It’s FDA-cleared, non-invasive, and has fewer side effects than other options, like antidepressants or ECT.
- The most common side effects of TMS include a tingling sensation, pain at treatment site, headaches, and neck or jaw pain. Most disappear shortly after a session, and your TMS team can help minimize these effects.
- While TMS is safe and effective for most people, it’s not recommended for those who have any metal-containing implants in their brain, such as a cochlear implant or metal plate. People with a history of seizures or epilepsy or severe headaches may also not be the best candidates for TMS.
- Before starting TMS, discuss any potential side effects, risks, and benefits with a psychiatrist experienced in this treatment, such as the team at Radial. They can help you decide if this is the right treatment for you.
Frequently asked questions (FAQs)
Can TMS cause memory loss?
TMS does not cause memory loss. In fact,early findings suggest it may improve memory.
Can TMS cause brain damage?
No. There is no evidence that TMS causes brain damage. This FDA-cleared mental health treatment is noninvasive with relatively few side effects.
Is TMS dangerous?
TMS is not dangerous. It’s a FDA-cleared, noninvasive procedure with fewer side effects than other options, like antidepressants and ECT. Before undergoing TMS many people ask, “does TMS therapy hurt?” While some people experience mild pain or a tingling sensation during or right after treatment, it disappears quickly and is less common as sessions progress.
Can TMS make tinnitus worse?
Without ear plugs or protection for the ears, the loud clicking noises of the TMS machine may cause hearing issues, including making tinnitus worse. The risk of this is low, especially if someone gets treatment at a clinic like Radial where we use hearing protection and there are trained technicians and a psychiatrist to oversee treatment. In fact, researchers are exploring if TMS may even be used to treat chronic tinnitus when delivered safely by trained technicians.
Can TMS make you tired?
Some people report feeling tired or fatigued immediately after a session. This isn’t a common side effect, and if it occurs, it usually goes away on its own.
Deep dive recommendations
- Radial. What is TMS?
- The Frontier Psychiatrists. What Are the Side Effects of Transcranial Magnetic Stimulation (TMS) Treatment?
- Metabolic Mind Podcast. The Truth About Treatment-Resistant Depression: Part Two (TMS and Psychedelics).
- Psychiatry Research. Safety and efficacy of Deep TMS for adolescent depression based on large real-world data analysis.
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started




