What Is Postpartum Rage? Understanding Anger After Birth

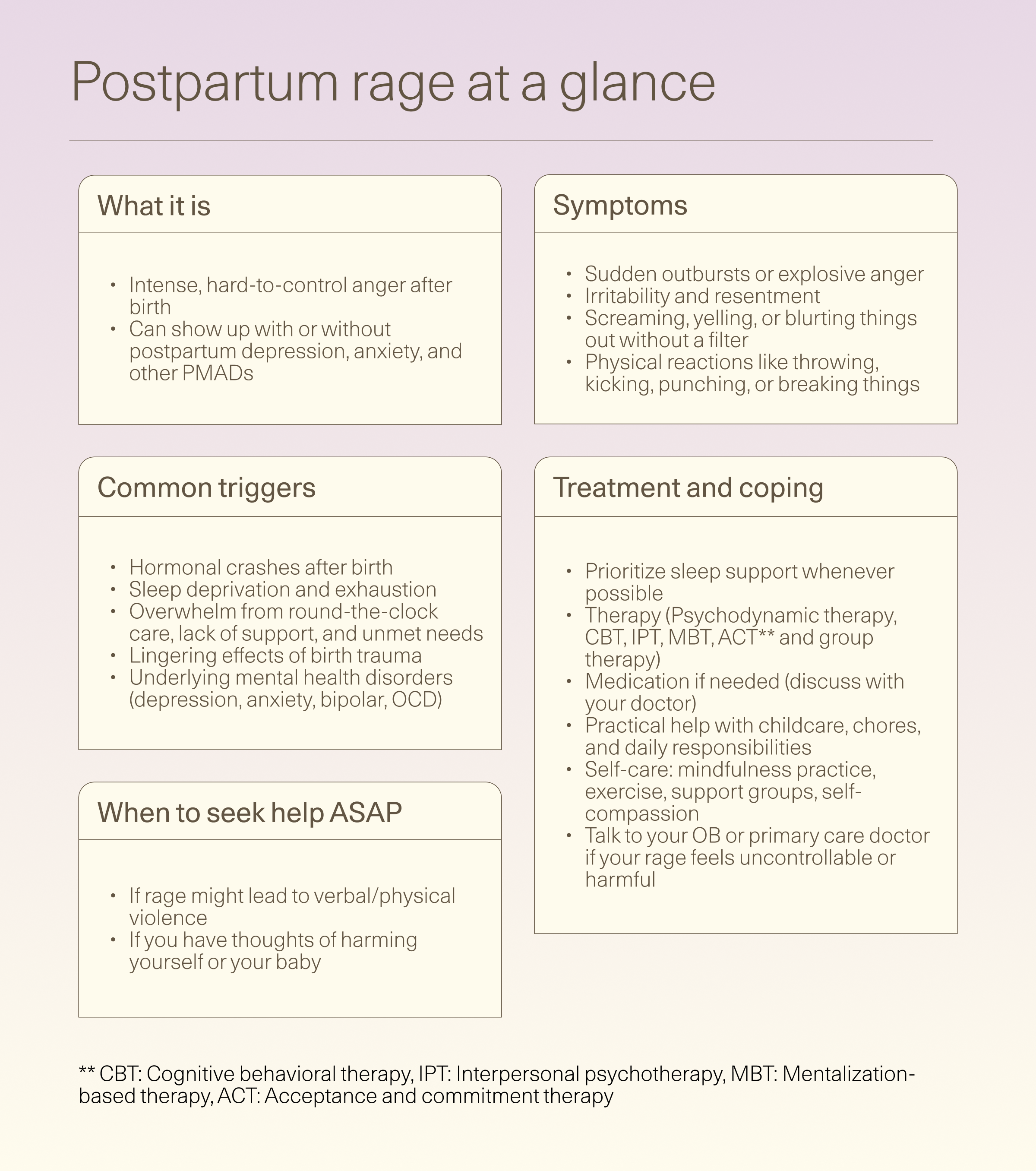
Feeling like your temper is shorter than ever after having a baby? That intense, hard-to-control anger might be postpartum rage—and understanding what’s behind it is the first step to finding relief.
Postpartum rage isn’t something most of us hear about during pregnancy, but for many new parents, it’s a very real (and very overwhelming) part of life after birth. I know because I lived it. After a complicated pregnancy, a scary premature delivery, and a rough recovery, I thought the hardest part was behind me. But once I was home—sleep-deprived, still healing, and buried under round-the-clock feedings—I was blindsided by an anger I couldn’t explain. It felt like hot lava coursing through my body, ready to erupt at any time.
Even with a supportive partner, I felt consumed by resentment. There was no time to heal, no time to shower, no time to just breathe. And then came the guilt: I should be savoring baby snuggles and that sweet newborn smell, right? Instead, I felt like I was the only new mom drowning in anger.
What I didn’t realize at the time is that I was experiencing postpartum rage, a form of intense, hard-to-control anger that often goes overlooked, but is likely more common than people think. If you’re searching for answers about how to deal with postpartum rage, rest assured you’re not alone. This guide breaks down what postpartum rage looks like, why it happens, and how to find the support and strategies that can help.
What is postpartum rage?
Postpartum rage isn’t just being cranky—it’s “an intense, short-lived, disproportionate” burst of anger that can feel completely out of control, says Stephanie Hartselle, MD, board-certified pediatric and adult psychiatrist and diplomate of the American Board of Psychiatry and Neurology.
While everyone experiences moments of fierce anger here and there, it becomes a problem if a recurring pattern of intense rage starts to affect your life, relationships, and mental health.
Currently, “postpartum rage is not a clinical diagnosis,” Dr. Hartselle explains. In fact, there are very few studies that even mention the term.
What we do know: rage may be linked to other perinatal mood and anxiety disorders (PMADs), she says. PMADs are a spectrum of mental health conditions that can show up during pregnancy and after childbirth. They’re different from the short-lived “baby blues,” which usually fade within two weeks.
According to Dr. Hartselle, postpartum rage can be a symptom of PMADs like:
- Postpartum depression: persistent sadness, loss of interest or pleasure, and feelings of worthlessness
- Postpartum anxiety: excessive worry, restlessness, and intrusive thoughts
- Postpartum bipolar disorder: cycles of depression (low mood, low energy) and mania. Manic episodes often present differently in the postpartum period, with symptoms like anxiety, confusion, mental fatigue, and rapid mood changes.
- Postpartum obsessive compulsive disorder (OCD): repetitive, unwanted, intrusive thoughts (obsessions) and irrational, excessive urges (compulsions) related to the health and safety of the baby
- Postpartum psychosis: rare but severe; presents with hallucinations, delusions, and cognitive symptoms like disorientation
- Postpartum post-traumatic stress disorder (PTSD): often develops after a traumatic birth experience; symptoms include intrusive memories, avoidance of trauma reminders, anxiety, and increased arousal
While postpartum rage may be a symptom of other conditions like depression, early evidence suggests it might be a distinct issue (and an under-recognized PMAD). Some research also links intense maternal anger to poor sleep quality for both mother and baby—suggesting rage is not necessarily just a “symptom”, but rather a condition that develops in certain circumstances.
Diagnoses aside, new motherhood presents enough chaos to spark angry episodes in almost anyone. “Fragmented sleep, feeding demands, dramatic changes in circulating hormones, and recovery from the birthing process can all lead to understandable episodes of extreme anger and rage,” says Dr. Hartselle.
Just because research is limited doesn’t mean postpartum rage isn’t real—or deeply disruptive. If you’re experiencing postpartum rage, know this: you’re not alone, and it deserves attention and care.
How common is postpartum rage?
The short answer: it’s still unclear. “We don't know how common this is,” says Dr. Hartselle. With limited research, there simply aren’t solid stats yet.
Still, it may be more widespread than you’d expect. In one survey of 278 new moms, nearly a third (31%) reported experiencing intense anger.
And if postpartum rage is indeed connected to other mood disorders—like depression, anxiety, or bipolar disorder—we can make some educated guesses. For context, postpartum depression affects an estimated 10–20% of women, while postpartum anxiety impacts about 10–15%.
And even for women with no prior psychiatric history, the perinatal period can bring unexpected challenges: around 2.6% develop bipolar disorder, and as many as one in six experience OCD symptoms, often overlapping with depression.
Without more research, though, we can’t say exactly how common postpartum rage is. But the evidence we have suggests it’s not rare, and more data is sorely needed.
What are signs and symptoms of postpartum rage?
Postpartum anger can show up in different ways depending on the person. Common postpartum rage symptoms and signs include:
- A short fuse or overwhelming anger—often directed at a partner, children, yourself, family members, or even healthcare providers
- Feeling out of control or battling aggressive urges
- Screaming, yelling, or blurting things out without a filter
- Physical reactions like throwing, kicking, punching, or breaking things
- Intrusive thoughts of violence
- Regret, shame, or confusion after an episode (for example, feeling guilty for getting angry with the baby)
Not all postpartum rage looks like yelling or throwing things. Some moms keep it bottled up, stewing silently while the anger simmers inside. But pushing those feelings down often makes things worse, fueling even more postpartum irritability when needs remain unmet, according to a qualitative study of new moms.
Rage can also show up physically. In the same study, new moms described it as a full-body experience: shaking, burning sensations, feeling “hot” and “heavy” in the chest or head, or feeling their “blood boiling.”
If you or someone you love is having outbursts of anger that feel out of character—especially if they involve verbal or physical aggression—it’s important to flag it with your OB or primary care doctor right away, says Dr. Hartselle. Even if it doesn’t meet the criteria for a diagnosable disorder, it’s still a clear sign that more support is needed. A doctor can help connect you with resources, monitor for underlying conditions, and ensure both parent and baby get the care they deserve.
What causes postpartum rage?
If you’ve felt blindsided by postpartum aggression, you’re not alone. It often stems from a mix of shifting hormones, sheer exhaustion, the overwhelming demands of new parenthood, and many more factors. Here’s what we know so far about what contributes to postpartum rage.
Hormonal changes
Your hormones don’t just dip after birth—they fall off a cliff. Estrogen and progesterone levels plummet, and those shifts can mess with neurotransmitters like serotonin and dopamine (a.k.a. your brain’s mood regulators). When those chemicals are out of balance, postpartum depression, anxiety, and other mood disorders can develop.
Researchers are also looking beyond estrogen and progesterone and their effects on serotonin. A drop in neurosteroid hormones—molecules that help send signals between cells—may also play a role in postpartum mental health. One neurosteroid in particular, allopregnanolone, rises during pregnancy to protect the baby’s brain from stress hormones. But after delivery, its job is done, so levels crash.
Here’s why that matters: allopregnanolone influences the brain’s gamma-amino butyric acid (GABA) receptors, which act like tiny brakes to calm overactive nerve cells. When allopregnanolone levels drop, those “brakes” don’t work as well, potentially leading to more anxiety and depression.
Still, science doesn’t yet understand the full picture of how and why PMADs develop. Hormones clearly influence postpartum mood, but researchers are still piecing together exactly how these shifts spark symptoms like postpartum rage.
Sleep deprivation
Night after night of broken sleep, endless feedings, and a baby who refuses to settle can leave you running on fumes—and fuming. In one qualitative study, new moms said lack of sleep was the number-one physical need that, when unmet, left them on edge and prone to explosive anger.
Some experimental research shows even non-postpartum people get angrier and more reactive when sleep-deprived. So imagine stacking that exhaustion on top of the demands of a newborn: it’s a perfect storm for irritability, frustration, and rage.
Even more concerning, poor sleep can raise the risk of suicidal thoughts and behaviors during the peripartum period. Research shows women with depression or other psychiatric conditions are especially vulnerable, but sleep problems alone more than double the odds of suicidal ideation, and insomnia triples the rate of postpartum suicide attempts.
The takeaway: sleep disturbances aren’t just an annoyance; they’re a serious health risk. That’s why screening for—and treating—sleep problems during pregnancy and postpartum is crucial for protecting both mental health and safety.
Stress overload
The perinatal period (pregnancy through the first year postpartum) is packed with massive life changes and new stressors. This makes it a particularly vulnerable time, putting you at risk for postpartum mood disorders.
Then, add in financial worries, relationship strain, or other major upheavals, and stress levels skyrocket, further increasing your odds of postpartum mental health struggles like postpartum rage. Research shows high maternal stress can make it harder to regulate emotions—so anger rises to the surface faster.
When you layer stress on top of hormonal shifts and chronic sleep deprivation, it’s no wonder many new moms feel overloaded, overwhelmed, and constantly on edge.
Socioeconomic pressures
Postpartum mood and anxiety disorders are often tied to socioeconomic disadvantage, and anger has been specifically linked to financial strain. For mothers in lower-income households, the stressors pile up:
- The financial burden of caring for a newborn when money is already tight
- Limited access to healthcare and postpartum support services
- Limited or no access to paid maternity leave, returning to work soon after birth
- Challenges finding or paying for childcare that matches working hours
These pressures compound the risk of mood disorders, heighten stress, and leave parents more vulnerable to frustration and rage.
Lack of support
They say it takes a village to raise a child, but what happens when the village is missing? Social support is crucial in the postpartum period, both emotionally and practically. Without enough help from partners, family, or friends, many mothers feel isolated and overwhelmed.
Research shows unmet expectations of support often fuel maternal anger. When partners or relatives don’t step up—whether it’s helping with nighttime feedings or simply allowing new moms to rest—frustration quickly boils over. The combination of unmet needs, exhaustion, and disappointment can turn simmering stress into full-blown rage.
Mental health conditions (past and present)
Your mental health history doesn’t disappear when you have a baby, and for many women, it raises the stakes. Those with a history of depression, anxiety, or other mental health conditions are more vulnerable to postpartum mood disorders. Same goes for people dealing with a pre-existing mental health issue.
Some conditions carry particularly sharp risks. For instance, women with bipolar disorder face a higher likelihood of developing postpartum mood symptoms—including anger and rage.
Past trauma
For some birthing people, postpartum rage is tied to old wounds. “We do understand that postpartum anger or rage can be increased in likelihood by those with a history of PTSD,” says Dr. Hartselle.
Pregnancy, childbirth, and early parenting can trigger trauma symptoms, often making them worse. For some trauma survivors, the perinatal period is filled with reminders that make a past trauma feel like it’s happening again. For example, vaginal exams may trigger memories of a past sexual assault, or interactions with dismissive providers may stir up feelings of helplessness from childhood.
When these traumatic reminders resurface, they can trigger rage. PTSD itself includes symptoms like irritability, aggression, and negative mood—and when layered with postpartum stressors like sleep deprivation and the worry that comes with caring for a fragile newborn, anger can intensify, says Dr. Hartselle.
Complicating matters more, a history of trauma also increases a person’s risk of experiencing a traumatic birth—in fact, research suggests a third of births in the United States are considered “psychologically traumatic.” The cascade effect of past trauma into birth trauma can set anyone up for feelings of rage and despair.
Violated expectations and compromised needs
Recent qualitative research highlights two big drivers of postpartum rage: unmet expectations and neglected needs.
- Violated expectations: Many new moms enter parenthood with certain assumptions—for example, how much support they’ll have from partners or family, or how quickly they’ll learn to breastfeed. When reality differs from expectations, the result can be frustration and anger.
- Compromised needs: What’s more, moms often can’t meet their own basic needs. Sleep, proper nutrition, rest, and self-care become luxuries. A loss of autonomy (no time for hobbies, work, social connection, or personal fulfillment) and unmet needs for love or connection can compound, building resentment.
Put together, these disappointments create fertile ground for rage, especially when layered with the enormous physical, emotional, and hormonal shifts of postpartum life.
Who gets postpartum rage?
Pregnancy, birth, and new parenthood are massive stressors that can leave anyone more vulnerable to intense anger. “Giving birth is one of the most wonderful and dangerous events of a mother’s life,” says Dr. Hartselle. “Regardless of age or health status, it’s an enormous tax on the body in terms of physical trauma, emotional exhaustion, and hormonal changes.”
Risk factors for developing postpartum rage
The main risk factors for developing postpartum rage are similar to the risk factors for perinatal mood disorders, and may include:
- Existing mood disorders
- Sleep deprivation
- History of trauma
- Emerging symptoms of bipolar disorder
- Lack of social and emotional support
- Socioeconomic challenges
- Lack of culturally competent care
- Genetic predisposition
Recognizing these risk factors helps providers catch warning signs early and offer appropriate treatment. The goal isn’t just to treat PMADs and postpartum rage after they surface, but to prevent them—and to give every new parent the support they need for a healthier start.
How long does postpartum rage last?
If you’re in the throes of intense postpartum mood swings, you might be desperate to know: How long does postpartum rage last?
The truth is, we don’t really know because it hasn’t been studied much at all, says Dr. Hartselle.
That said, we can guess from related disorders. Since postpartum rage often overlaps with other mood disorders like depression, anxiety, or bipolar disorder, experts may look to those conditions for clues about onset and duration. “Postpartum disorders such as depression and bipolar disorder typically declare themselves within several weeks of giving birth,” explains Hartselle.
The timeline for recovery is dependent on whether the underlying causes are treated effectively. “Recovery depends on what drives the rage,” says Hartselle.
- If postpartum rage is due to sleep deprivation and exhaustion, anger often eases once parents get consistent rest and support with feeding or baby care, Hartselle says.
- If postpartum rage is a byproduct of depression, anxiety, or mania, recovery depends on working closely with a healthcare provider to find safe, effective treatments that protect both the parent’s and baby’s well-being, she says.
How is postpartum rage diagnosed?
Postpartum rage isn’t an official diagnosis. That means there’s no formal criteria to identify it, and health professionals must listen to the experiences patients mention in their intake.
But, since rage often shows up alongside PMADs, screening for those conditions can be a critical first step. Clinicians have several evidence-based tools to identify PMADs:
- Edinburgh Postnatal Depression Scale (EPDS): Screens for depression, anxiety, and suicidal thoughts.
- Patient Health Questionnaire (PHQ-9): Focuses on depression and suicidal ideation; mirrors DSM criteria.
- Mood Disorder Questionnaire (MDQ): Helps spot bipolar disorder.
- Generalized Anxiety Disorder scale (GAD-7): Screens for anxiety symptoms.
- Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Assesses post-traumatic stress.
- Postpartum Depression Screening Scale (PDSS): measures symptoms of postpartum depression.
Still, early research suggests that anger can sometimes appear as its own distinctive perinatal mood symptom, even without signs of depression, for example. That’s why many experts argue clinicians should be screening for rage directly when assessing PMADs.
Of course, it’s not just about which tools providers use—it’s also about when they use them. Screening tools are only useful if they’re used at the right times. Best practice guidelines recommend checking in at multiple points across pregnancy and postpartum, since symptoms can emerge or worsen at different stages. Suggested screening windows include:
- First prenatal visit
- At least once during the second trimester
- At least once during the third trimester
- Six-week postpartum visit (or at the first postpartum visit)
- Repeat screenings at 6 and/or 12 months in OB and primary care visits
- Pediatric visits at 1, 2, 4, and 6 months
Regular, repeated screening increases the chances of catching issues early before they escalate. OB-GYNs, midwives, primary care providers, and mental health professionals play a key role in prevention and support. By educating families about postpartum mood disorders, dispelling myths, and reducing stigma, providers can encourage more open, honest conversations. And when new moms feel safe to speak up, they’re far more likely to get the care and support they need.
How is postpartum rage treated?
Sometimes postpartum rage isn’t tied to a specific mental health disorder—it may stem from sleep deprivation, lack of support, or the stress of adjusting to new parenthood. In those cases, treatment starts with practical help: connecting parents to resources, education, and support systems that can ease the load, says Dr. Hartselle.
But when rage is linked to PMADs, treatment focuses on addressing the underlying condition. Getting the right diagnosis might not sound exciting, but it’s the foundation of effective postpartum rage treatment, says Dr. Hartselle.
Common treatment options for PMADs include:
Therapy
Evidence-based therapeutic approaches are proven to help those experiencing postpartum mood disorders. Some of these are:
- Cognitive behavioral therapy (CBT): helps identify and reshape negative thought patterns, giving you healthier coping skills and strategies.
- Interpersonal psychotherapy (IPT): focuses on strengthening relationships and resolving conflict, since social support plays a huge role in recovery.
- Psychodynamic therapy: helps you identify how unconscious thoughts, desires, and memories may influence behavior.
- Acceptance and commitment therapy (ACT): helps you accept tough thoughts and feelings instead of fighting them, while staying focused on living by your core values.
- Mentalization-based therapy (MBT): teaches you to notice how your thoughts and feelings shape your actions—and how they affect the people around you—so you can better understand yourself and others.
- Group therapy: offers valuable peer support while also helping you learn proven strategies for coping.
Beyond techniques, therapy provides something equally valuable: a safe space to process emotions, improve communication, and learn stress management tools.
Medication
While there’s no specific “postpartum rage medication,” antidepressants—most often selective serotonin reuptake inhibitors (SSRIs)—are another frontline treatment for PMADs like postpartum depression. SSRIs boost serotonin, a brain chemical tied to mood, sleep, and stress. They can take a few weeks to work and help roughly 40-55% of patients.
If medication is an option, it’s best discussed with a provider who can weigh risks and benefits for both mom and baby. While there is some degree of risk associated with taking medication when pregnant or breastfeeding, it’s crucial to remember there are serious risks to PMADs left untreated.
Two newer FDA-approved neurosteroid drugs specifically target postpartum depression:
- Zuranolone: a daily pill for two weeks that can start working within days. It acts on GABA-A receptors, helping to regulate hormones (instead of serotonin).
- Brexanolone: an IV infusion over 60 hours in a hospital, working in a similar way to zuranolone.
Both have shown meaningful improvements on clinical depression scales.
Medication-related risks
Though medications can be life-changing for some, no drug is risk-free:
- Risks of SSRIs: In some studies, use of traditional antidepressants during pregnancy was associated with certain birth defects (venlafaxine in particular has raised red flags, though more research is needed), pregnancy-induced hypertension, and other complications such as lower birth weight, neonatal withdrawal symptoms, and postpartum hemorrhaging.
- Risks of Zuranolone: Promising but too new for us to know long-term effects. Short term side effects include sleepiness and dizziness. Questions remain about safety while breastfeeding and addiction potential.
- Risks of Brexanolone: Effective but impractical for many—it requires hospitalization and comes with a high price tag. Side effects are similar to zuranolone, along with possible loss of consciousness.
Transcranial magnetic stimulation (TMS)
Transcranial magnetic stimulation (TMS) is gaining attention as a non-drug option for perinatal depression. Using magnetic fields to stimulate brain regions tied to mood, TMS has shown meaningful reductions in depression symptoms during pregnancy and postpartum.
The upside:
- Noninvasive and chemical-free, so no drug exposure for mom or baby
- Generally well tolerated, with minimal side effects compared to antidepressants or electroconvulsive therapy (ECT).
The caveats:
- Risk of seizure (less than 1%, but still the most serious concern)
- Long-term effects of fetal exposure to magnetic fields remain unknown, though current data suggests exposure levels are well below safety thresholds
Even with those unknowns, early evidence suggests TMS could be a safe and effective alternative for people who can’t—or don’t want to—use medication. Want to learn more? The experts at Radial are here to help you access fast-acting, cutting-edge, evidence-based treatments that meet you where you are—virtually or in-person.
Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) often carries a stigma, but it’s one of the most effective depression treatments available. The procedure uses controlled electrical impulses to trigger a brief seizure while under general anesthesia.
Despite its reputation, studies show ECT is relatively safe during pregnancy, especially for women with severe symptoms like suicidality, psychosis, or mania. According to the current data, miscarriage rates don’t appear higher than in the general population, and no links have been found to birth defects or long-term neurocognitive issues in children.
That said, risks still exist: anesthesia complications, memory loss, induced seizures, or preterm contractions (though it’s still unclear if ECT is the cause). With safety precautions in place (such as fetal monitoring during the procedure), many of these risks can be managed. Ultimately, ECT is a matter of weighing risks against the dangers of leaving severe psychiatric symptoms untreated.
Peer support
Sometimes the most powerful medicine is simply not feeling alone. For new moms dealing with PMADs and/or postpartum rage, peer support groups offer a safe, judgment-free space for parents to connect, swap stories, and share coping strategies. The result? Less isolation, more validation, and a stronger sense of community.
For many, peer groups are a lifeline—reminders that their struggles are real, shared, and survivable.
What are realistic coping strategies for postpartum rage?
Postpartum rage can feel explosive, but there are ways to manage it before it boils over. The key is finding realistic strategies that help you cool down in the moment and build resilience for the long run. Here are some things you can actually do to help with postpartum rage.
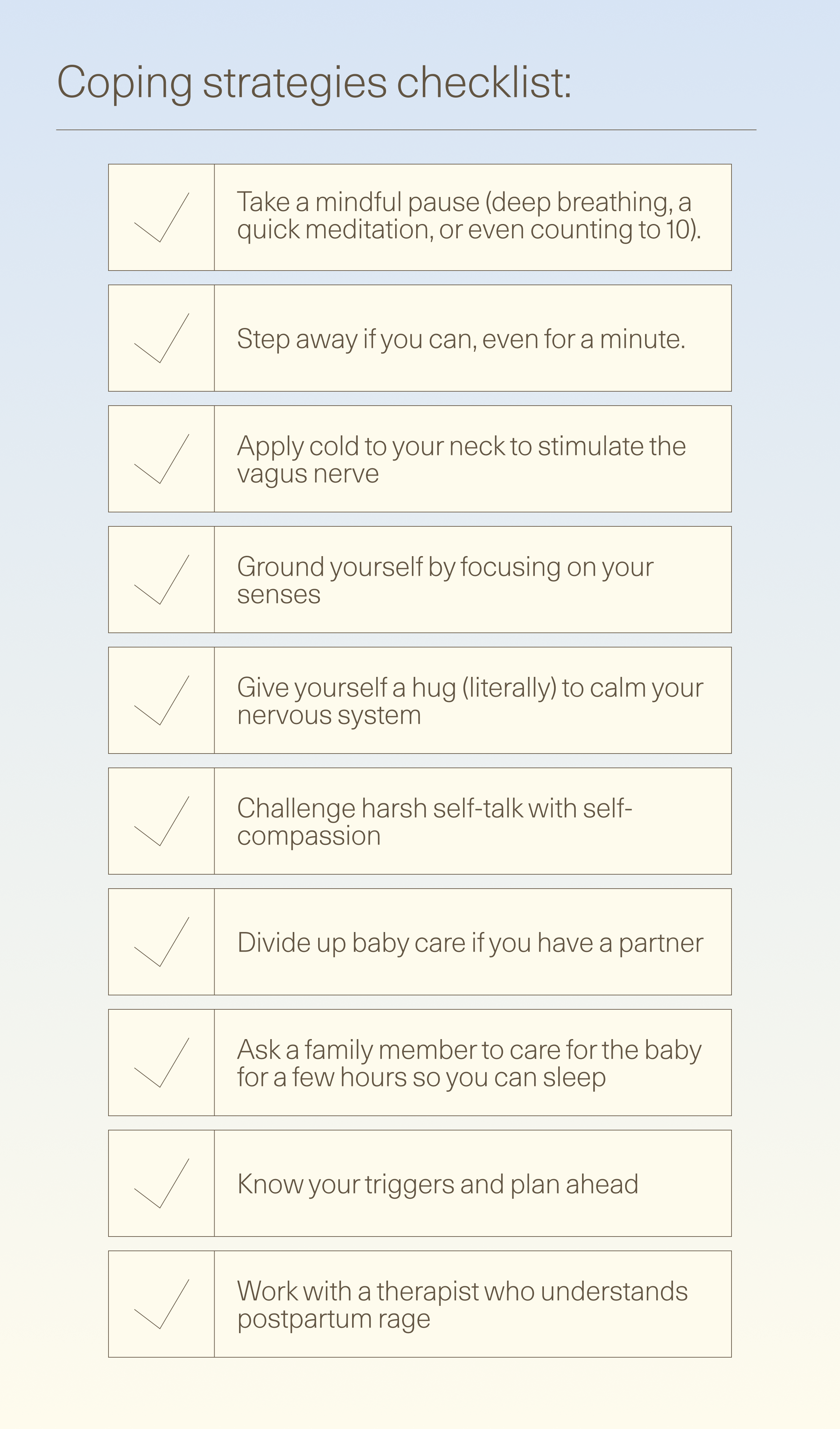
Practical ways to manage the heat of the moment
When rage begins to bubble, trying some of these coping strategies can help bring your temper back from the brink:
- Take a mindful pause. Research on anger shows deep breathing, a quick meditation, mindfulness-based interventions, or even counting to 10 can help your body shift out of high-alert mode. Even a minute of slow, deep breaths can help.
- Step away if you can. Go for a short walk (even in your backyard), hop in the shower, or simply move into another room to create some space.
- Ground yourself when you can’t leave. Focus on your senses—for example, the feel of the floor beneath your feet, the texture of carpet or tile—and pair it with slow, steady breaths. This helps you shift from feeling the rage inside to being aware of the here-and-now.
- Use cold to calm.Applying something cold to your neck can help stimulate the vagus nerve, which promotes relaxation.
- Switch gears. Open a window, play music, sip cold water. Small shifts in your environment can reset your nervous system.
- Give yourself a hug (literally). Wrapping your arms around your chest or placing a hand on your heart can send calming signals to your body.
Shifting your mindset and routines
- Challenge harsh self-talk. Experiencing rage doesn’t make you a “bad mom.” Self-compassion helps you respond with care rather than judgment. Think: This is hard. I’m doing the best I can.
- Share the load. Taking turns with night feeds or dividing baby duties can help ease exhaustion and resentment.
- Know your triggers. For example, if long stretches alone with the baby set you off, plan ahead: ask a friend to babysit, or join a parent-and-baby class for built-in company.
- Work with a therapist who understands postpartum rage. Having professional support from someone who “gets it” can make all the difference.
Whatever strategy works for you, the important thing is to release anger in a healthy way. Otherwise, you risk building pressure like a kettle ready to blow—something that can take a real toll over time.
How can I help someone with postpartum rage?
The best way to support a new mom dealing with postpartum rage is simple: show up and pay attention.
Start by giving her space to share what she’s feeling and what she needs. Dr. Hartselle recommends asking gentle, open-ended questions like:
- How do you experience these moments of anger?
- What do you think triggers them?
- What could I (or others) do to make things easier?
It’s also important to tune into her overall mood and behavior. If you notice signs of profound sadness, hopelessness, withdrawal, irrational worries, or behavior that feels out of character, encourage her to seek professional help, says Dr. Hartselle. Offer to support her in making that first step (like reaching out to her OB-GYN or primary care provider).
Support isn’t only emotional. Practical help goes a long way, too. Partners can take a night shift or early-morning feeding. Family and friends can drop off meals, throw in a load of laundry, or tidy up the kitchen. Qualitative research shows that moms who feel supported often cope better with anger, so even small gestures matter.
Keep checking in, keep showing up, and keep letting her know she’s not alone. That’s how to help postpartum rage feel less all-consuming and scary for a person you love.
When should I seek help?
Everyone gets angry sometimes, but rage that feels out of character, extreme, or unsafe is a red flag.
If a mom is having explosive outbursts—especially involving verbal or physical aggression—Dr. Hartselle stresses that this should be brought to her OB-GYN or primary care doctor right away. Other warning signs include rage paired with ongoing sadness, despair, compulsive worry, or withdrawal from loved ones.
Even if the anger doesn’t meet criteria for a clinical disorder, it’s often a clear signal that more support is needed, says Dr. Hartselle. A doctor can help assess whether treatment is necessary and connect families with resources to ease the pressure.
If rage is present without other concerning symptoms, loved ones can still step in with practical support (like taking over some feedings, giving mom more breaks, or simply making sure she gets rest), says Dr. Hartselle.
For new parents with intense rage: don’t brush off troubling feelings or try to “power through.” Left untreated, maternal mental health struggles can escalate to serious outcomes, including overdose and suicide, which are leading causes of postpartum death, says Dr. Hartselle.
If you're in a crisis, don’t wait. Support is one call, text, or click away.
If you're in a crisis, don't wait. Support is one call, text, or click away. Call 911 for immediate medical or safety emergencies. Call or text 988 (or chat online
to connect with a trained mental health crisis counselor at the Suicide and Crisis Lifeline.
Support and resources
Postpartum rage can feel like a storm you can’t control, but you don’t have to weather it alone. Real help is out there, and connecting with the right support can make all the difference.
If you or someone you know is struggling, reach out:
- Postpartum Support International (PSI): Call 800-944-4773 or text for immediate support and local referrals. PSI also runs online support groups and has an online directory of perinatal mental health professionals so you can find qualified help near you.
- National Alliance on Mental Illness (NAMI): Call 800-950-6264 or text 62640 to connect with the free, confidential NAMI HelpLine. You’ll get one-on-one emotional support, reliable mental health info, and resources to help you or your loved ones manage tough challenges.
- Radial: Radial provides evidence-based treatments for people who haven’t found relief with traditional care. Some options can be prescribed online, while others require in-person visits. They offer virtual consults in more than a dozen states, plus specialized treatments at select Centers of Excellence. You may choose to start care virtually, then travel to the location that works best for you.
You don’t have to push through postpartum rage (or any PMAD) on your own. The sooner you reach out, the sooner you’ll feel less angry and alone.
The bottom line
Postpartum rage may feel scary, isolating, and out of control—but it’s not a life sentence, and it’s definitely not a reflection of your worth as a parent. With the right support, treatment, and community, things can get better.
If rage is disrupting your life, don’t wait to get help. Radial can connect you with licensed clinicians—virtually or in-person—who understand what you’re going through and offer the latest fast-acting, evidence-based treatments. Together, you’ll build a plan that puts your mental health first.
Because you don’t have to just “ride it out.” You deserve relief, and support is within reach.
Key takeaways
- Postpartum rage is real, and it’s more common than people think.
- It can show up as snapping, yelling, intrusive thoughts, or even physical outbursts.
- Hormonal crashes, exhaustion, and mood disorders like depression or anxiety can all fuel postpartum rage.
- Recovery depends on the cause: sometimes sleep and support help, sometimes medical or therapeutic treatment is needed.
- You don’t have to face postpartum challenges alone—support groups, therapy, and preventative medical care can make a huge difference.
Frequently asked questions (FAQs)
What are examples of postpartum rage?
Postpartum anger doesn’t show up the same way for everyone, but some common signs include:
- Snapping or losing your temper easily—often at a partner, kids, family, or even yourself
- Feeling out of control or struggling with aggressive urges
- Screaming, yelling, or blurting things out without a filter
- Physical reactions like throwing, punching, kicking, or breaking things
- Intrusive thoughts of violence
- A wave of guilt, shame, or confusion after an episode (like feeling guilty for snapping at your baby)
What is the biggest hormone drop in postpartum?
Estrogen and progesterone levels plunge right after delivery, and that crash can throw off brain chemicals like serotonin and dopamine, which regulate mood. When these neurotransmitters are out of balance, it can set the stage for postpartum depression, anxiety, and other mood disorders.
Neurosteroid hormones like allopregnanolone nosedive too, potentially leading to more anxiety, depression, and mood changes.
When does postpartum rage start?
There isn’t much research, but experts have some clues. Postpartum rage often overlaps with mood disorders such as depression, anxiety, or bipolar disorder. And those conditions usually surface in the first few weeks after giving birth, says Dr. Hartselle.
Deep dive recommendations and resources
- Psychiatry and Psychotherapy Podcast. 013: Postpartum Depression with Dr Pereau. Published April 24, 2018. https://podcasts.apple.com/us/podcast/013-postpartum-depression-with-dr-pereau/id1335892956?i=1000409689419
- Psychiatry and Psychotherapy Podcast. Episode 184: Pregnancy Planning for Patients Taking Psychiatric Medication or with a Mental Health History. https://podcasts.apple.com/us/podcast/psychiatry-psychotherapy-podcast/id1335892956?i=1000618111066
- Defeat Postpartum Depression | Postpartum Anxiety, Postpartum Psychosis, Postpartum OCD Podcast. Arielle Wozniak. https://podcasts.apple.com/us/podcast/defeat-postpartum-depression-postpartum-anxiety-postpartum/id1459517793
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started



