What Is Accelerated TMS? How It Works and Who It Helps

Depression relief usually takes weeks, but what if it didn’t? Accelerated TMS is a newer, fast-acting brain-based treatment that aims to deliver meaningful results in days, not months—and we’re breaking down how it works, who it’s for, and how it stacks up against other options.
If you’re reading this, there’s a good chance accelerated TMS isn’t your first stop—it’s the option you’re looking at after trying things that should have helped but didn’t, at least not enough. When you’ve cycled through medications and therapy yet you’re still struggling, the search for something that actually moves the needle can feel exhausting—and urgent.
I know what it’s like to keep showing up, doing the work, trying different clinicians, different approaches, different versions of “self-care,” and still feeling stuck. When relief is slow—or nonexistent—it’s natural to want the next step to work, and to work faster. That’s why so many people are now looking into accelerated TMS for depression.
But the information out there can feel overwhelming. SAINT TMS, iTBS, accelerated schedules, multiple sessions a day—seriously, what the heck does it all mean, and more importantly, does it matter for better results? This article is here to cut through the noise.
We’ll walk you through what accelerated TMS therapy really is, how it works, who it may help, how it compares to other treatments, and what the science does—and doesn’t—say so far. No hype, no pressure—just clear, compassionate guidance.
What is TMS?
Repetitive transcranial magnetic stimulation (rTMS or just TMS) is a noninvasive treatment that uses magnetic pulses to stimulate specific brain regions involved in mood regulation. It’s been FDA-cleared for treatment-resistant major depressive disorder (MDD) for over a decade (and more recently for obsessive compulsive disorder, aka, OCD, and smoking cessation).
Standard TMS for depression typically targets the left dorsolateral prefrontal cortex (l-DLPFC) using high-frequency stimulation (often 10 or 18 Hz), delivered once daily for between 20-45 minutes over six weeks. It’s two seconds on, and a pause of less than a minute. This pattern of stimulation acts directly on the neural circuits linked to depression. With this on-again, off-again stimulation TMS can help relieve symptoms, especially when medications haven’t worked.
Common types of TMS include:
- Deep TMS (dTMS): Uses a specialized H-coil to reach deeper brain structures
- Accelerated TMS: Packs multiple sessions into a single day to shorten treatment time
- SAINT® TMS: A highly personalized, accelerated approach guided by brain imaging plus an AI-algorithm.
- SWIFT dTMS: it’s Deep TMS, but accelerated! It doesn’t use an fMRI to guide the treatment, but is approved by FDA
What is accelerated TMS and how does it work?
Traditional TMS works really well for depression, but the daily, weeks-long schedule can be tough to manage, especially if you’re juggling work, childcare, or transportation.
Accelerated TMS solves that problem by delivering more than one TMS session per day, compressing weeks of treatment into days. The goal? Faster symptom relief without sacrificing effectiveness, and in some cases, potentially improving outcomes.
In recent years, the FDA has cleared several accelerated TMS protocols:
- SAINT TMS: Combines MRI-guided targeting with 10 brief TMS sessions daily over five days, for 50 total stimulations.
- BrainsWay SWIFT Deep TMS: An accelerated deep-TMS protocol delivered over six days, with five sessions per day. There are then 4 weeks in which two stimulations delivered per day on a single day.
Early research suggests accelerated TMS treatment can significantly reduce symptoms of depression (and OCD), with some studies showing patients with depression improving more quickly than with standard TMS treatment schedules. That said, this field is still evolving, and experts are actively refining how best to deliver it.
Case in point: scientists and clinicians continue to refine techniques to target the right brain area for treatment. Most TMS protocols aim for the DLPFC, but there are several ways to find that spot:
- 5.5 cm rule: The most widely studied method. Clinicians locate the motor “hot spot” that moves the left thumb, then measure 5.5 cm forward to reach the DLPFC.
- Beam F3 method: Uses personalized skull measurements to position the coil over the scalp area that typically corresponds to the DLPFC.
- MRI (magnetic resonance imaging) guided targeting:
- Structural MRI: A detailed picture of the brain’s structure–it “can help confirm that stimulation is reaching the intended brain area,” says Colleen A. Hanlon, PhD, an adjunct professor at Wake Forest School of Medicine and Vice President of Medical Affairs at BrainsWay.
- Functional MRI (fMRI): A “more advanced technique … still mostly used in research,” it “measures brain activity” (think: changes in blood oxygen levels) to map the target, says Dr. Hanlon.
While MRI-guided approaches may theoretically improve precision, the science isn’t settled. “In some situations, imaging can be helpful but not necessary,” says Dr. Hanlon. For example, during longer TMS sessions, “small head movements or coil shifts can affect accuracy,” she says. In this case, a structural MRI can come in handy. Still, there are plenty of workarounds.
“Many systems address this in other ways, such as using wider electric fields or helmet-like designs that allow natural movement while maintaining consistent targeting,” Dr. Hanlon explains. Meaning, advanced brain imaging isn’t required for successful accelerated TMS. “In most cases, standard targeting methods combined with modern TMS devices work very well,” she says. Outcomes have steadily improved as technology advances and clinicians gain experience, she adds.
iTBS: The technology behind accelerated TMS
Used in certain accelerated TMS protocols like SAINT, intermittent theta burst stimulation (iTBS) is a rapid-fire stimulation pattern that mimics the brain’s natural rhythms. It allows clinicians to deliver effective treatment in a fraction of the time.
While not all accelerated protocols rely exclusively on iTBS, it’s a favorite because it’s fast: sessions last 160 seconds to deliver 600 pulses, compared to 20–30 minutes for traditional TMS to deliver an equivalent dose.
iTBS works by increasing neural excitability and strengthening synaptic connections—effects that can last well beyond the session itself. Research suggests that higher total pulse doses and more frequent sessions may lead to stronger clinical benefits.
The SAINT protocol: the gold standard of accelerated TMS
The FDA-cleared Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT) protocol is currently the most intensive accelerated TMS approach for MDD.
Here’s what makes it stand out:
- Uses iTBS
- Delivers the same pulse dose as a six-week iTBS protocol—in a single day
- Runs for five consecutive days
- Total dose: 90,000 pulses (five times the conventional iTBS dose)
- Ten sessions per day, spaced 50 minutes apart
- Uses personalized functional MRI to pinpoint the optimal treatment target
In a small clinical study, 79% of patients reached remission during the four-week follow-up after just five days of SAINT treatment for depression—an eye-opening result that continues to fuel interest and research.
How effective is accelerated TMS?
The results to date are very promising. “Accelerated TMS has been shown to be highly effective for treating depression, with the main advantage being that results can be achieved in a much shorter time frame than traditional TMS schedules,” says Dr. Hanlon.
Here’s what the research tells us so far.
SAINT TMS:
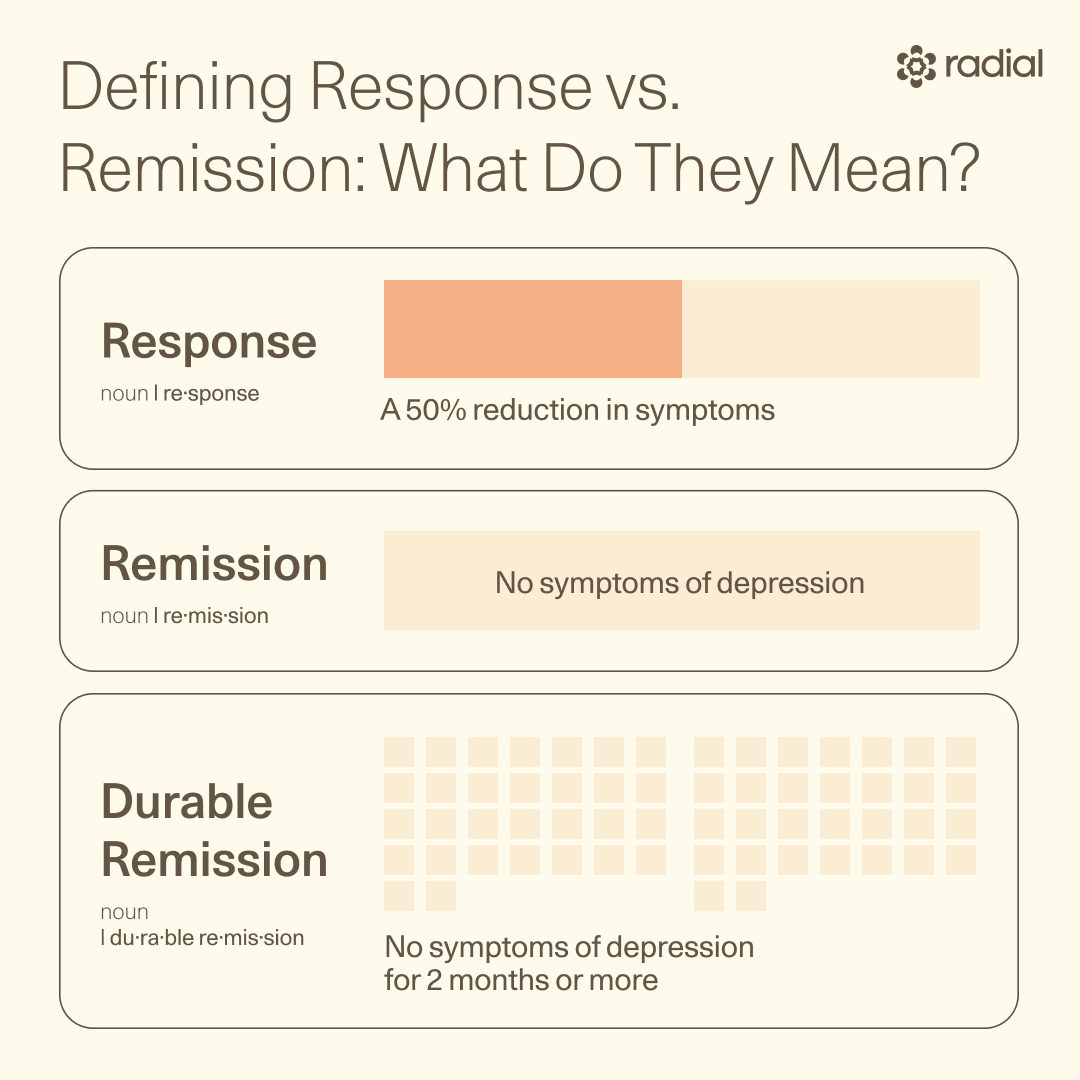
SAINT delivers some of the most striking early results. In a small clinical study, 79% of patients reached remission during the 4-week follow-up after just five days of treatment. In another SAINT study, 70% entered remission one week later, though durability dropped over time—about 33% remained in remission for depression at 12 weeks. In other words: fast relief, with ongoing questions about how long benefits last. However, with repeated treatments, patients were able to sustain or remission with no decrease in effect over time.
Accelerated Deep TMS:
Results here are also impressive. In an early case report, sequential bilateral theta burst deep TMS delivered strikingly fast results: one patient saw a 94% drop in depressive symptoms in just three days. Across patients, about half improved, and nearly 28% reached full remission in roughly 20 sessions—fewer than the usual 25–30 needed with traditional protocols.
Another retrospective study–co-authored by Radial’s chief medical officer and co-founder Owen Scott Muir, MD, DFAACAP–found that accelerated Deep TMS using the H1 coil led to an 80% response rate and 51% remission, with improvement starting as early as day 3 or 4. Even more encouraging, 93% of responders maintained benefits for six months.
Accelerated deep TMS also stacks up well against the traditional version. In one study, also co-authored by Muir, both accelerated and standard deep TMS protocols significantly reduced depression symptoms in people with major depressive disorder.
Similarly, a large multicenter trial of BrainsWay’s SWIFT Deep TMS protocol—including treatment at Radial—showed it “worked just as well as the standard deep TMS protocol,” but with “far fewer clinic visits,” says Dr. Hanlon, one of the authors of the study . “Response rates were nearly 88%, and remission rates were about 78%,” comparable to the standard protocol, she says. The key difference? Speed. Patients reached remission faster, with a median time of 21 days versus 28 days on the traditional schedule.
Despite the strong early data, accelerated TMS is still a developing field. Many studies so far have small sample sizes, varying methods, and different targeting approaches, which makes it hard to draw firm, universal conclusions.
Researchers are still figuring out important details—like the ideal number of sessions per day, the best spacing between sessions, and the total dose needed for lasting results. Until larger, more standardized studies are completed, experts agree the evidence is encouraging but evolving. Ongoing research will help clarify how to optimize treatment and how lasting the results truly are.
How does accelerated TMS compare to other treatments?
Accelerated TMS is a promising, science-backed option for depression, but it’s not the only one. Medications, standard TMS, and other therapies all have a role. The real question is how accelerated TMS stacks up in terms of speed, effectiveness, side effects, and access.
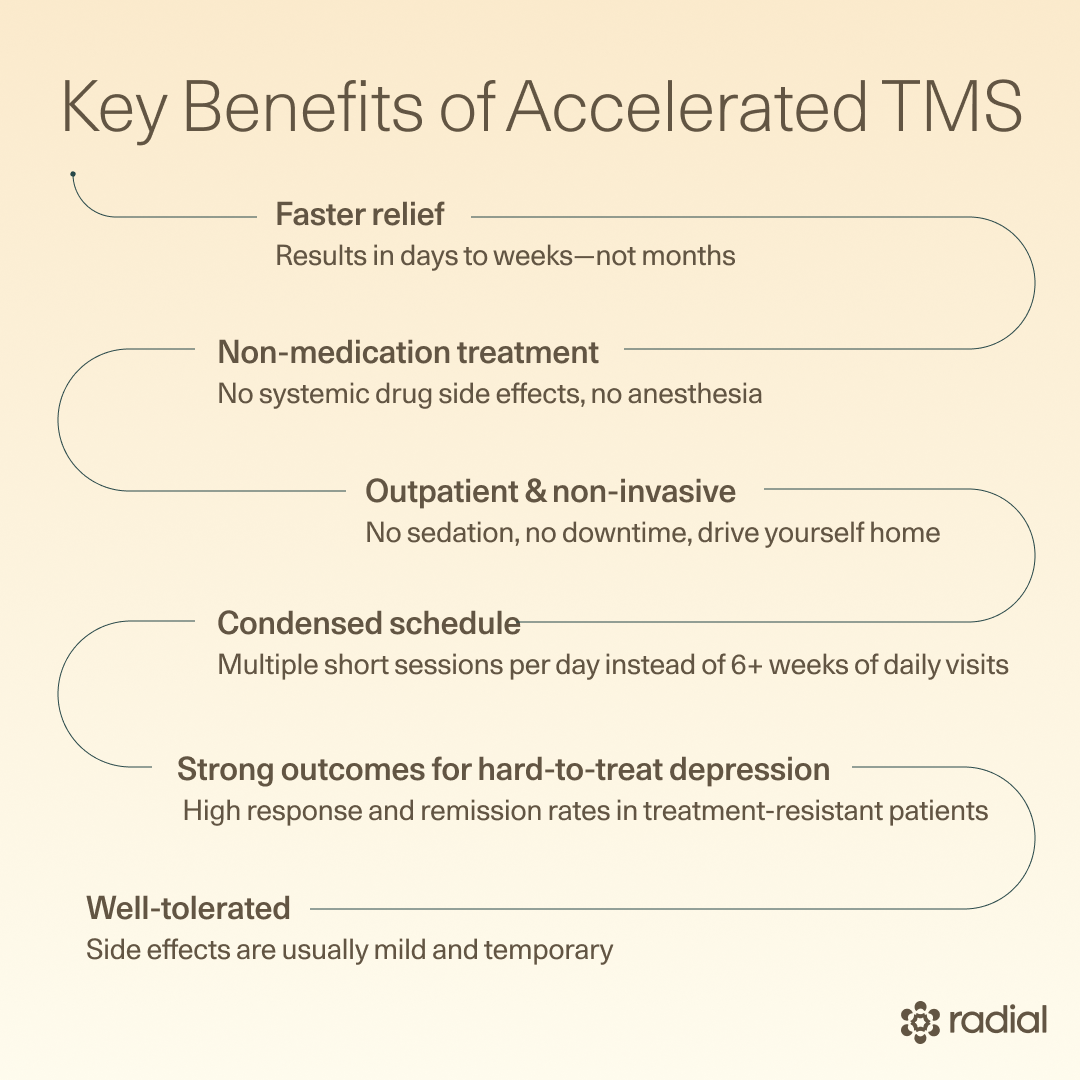
“Compared with other depression treatments, accelerated Deep TMS” and other accelerated protocols offer “a non-medication option with minimal side effects and no anesthesia,” says Dr. Hanlon. Accelerated TMS also boasts “strong clinical outcomes, faster relief, and a more convenient treatment schedule,” she adds.
Let’s break it down.
Accelerated TMS vs. standard rTMS
Same idea, very different pace. Both treatments stimulate mood-related brain circuits using magnetic pulses, but accelerated TMS compresses the timeline.
Treatment timeline
- Standard TMS: One session a day, five days a week, for 4–6 weeks
- Accelerated TMS: Multiple short sessions per day over just 5–6 days. For example:
- SAINT delivers a full six-week pulse dose in five days: 10 treatments per day for 5 consecutive days (a total of 50 treatments). Each session lasts about 5 minutes, 50 minutes apart.
- SWIFT Deep TMS: 5 treatments per day for 6 days over 2 weeks, then 2 treatments per day a week for 4 weeks (a total of 38 treatments). Each session lasts between 3-9 minutes, 50 minutes apart.
- ONE-D protocol: 20 treatments in 1 day. Each session lasts approximately 3 minutes and treatments are 30 minutes apart.
Effectiveness
- Early studies suggest accelerated TMS may reduce symptoms faster than standard TMS
- SWIFT Deep TMS shows response rates near 88% and remission around 78%, comparable to standard Deep TMS, but with quicker time to remission (about 21 vs. 28 days)
- SAINT data suggest antidepressant durability similar to conventional TMS (meaning, how long the positive effects last)
Side effects
- Very similar for both: typically mild, temporary, and manageable (headache, scalp discomfort, fatigue)
FDA status
- Standard TMS is FDA-cleared
- Some accelerated protocols (including SAINT and BrainsWay’s SWIFT Deep TMS) are also FDA-cleared for treatment-resistant depression
Insurance coverage
- Standard TMS is usually covered after multiple medication failures
- Accelerated TMS may be covered in select cases, depending on medical necessity and your plan
Important caveat: While early results are encouraging, fewer studies directly compare accelerated and standard TMS head-to-head. Researchers are still refining the “sweet spot” for sessions per day, spacing between sessions, and total pulse dose.
Accelerated TMS vs. antidepressant medications
Antidepressants are often the first stop, but they’re not the best fit for everyone.
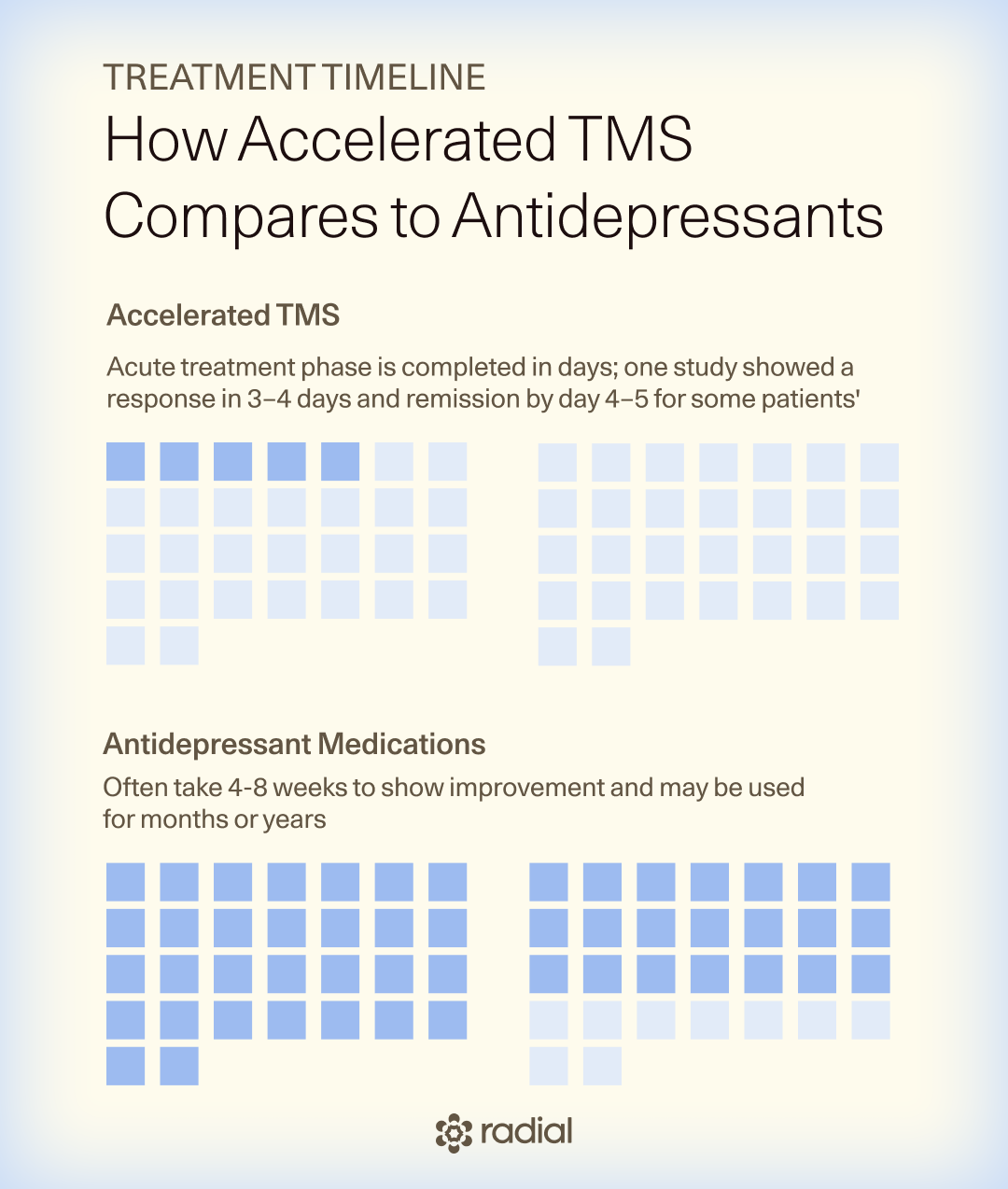
Treatment timeline
- Medications: Often take 4-8 weeks to show improvement and may be used for months or years
- Accelerated TMS: Acute treatment phase is completed in days; one study showed a response in 3–4 days and remission by day 4–5 for some patients
Effectiveness
- About 30% of people with MDD don’t respond to antidepressants
- Accelerated TMS shows high remission rates in treatment-resistant depression (up to 79% in SAINT studies; 80% response with accelerated Deep TMS)
Side effects
- Antidepressants: Can include nausea, weight gain, sleep issues, and sexual side effects
- Accelerated TMS: Typically limited to short-term scalp discomfort, headaches, or fatigue—no systemic effects
FDA status
- Many antidepressants are FDA-approved
- Select accelerated TMS protocols are FDA-cleared for treatment-resistant depression
Insurance coverage
- Antidepressants are widely covered
- Accelerated TMS coverage varies and often requires documentation that medications didn’t help
Accelerated TMS vs. ketamine / esketamine
Like accelerated TMS, fast-acting medications ketamine and esketamine (a derivative of ketamine) work quicker than traditional antidepressants, but they work differently.
Treatment timeline
- IV ketamine: Usually starts with a series of 3 infusions over a few weeks to see if it helps. If it does, patients often continue with another 3–5 sessions and many require ongoing maintenance.
- Esketamine (brand name Spravato): Typically given twice weekly for the first 4 weeks, then weekly for another month and every other week after that for maintenance.
- Accelerated TMS: Multiple short sessions per day over just 5–6 days. Some protocols involve several weekly sessions after the acute treatment phase.
Effectiveness
Ketamine and esketamine can work fast—often within 24 hours. Studies suggest esketamine leads to about 37–40% remission and 48–60% response after the first month. The catch? The antidepressant effect often fades, making maintenance treatments common.
Accelerated TMS shows higher remission rates in treatment-resistant depression—up to 79% in SAINT studies and 80% response with accelerated Deep TMS. In one observational, head-to-head study, accelerated TMS produced faster and stronger responses at one month compared to esketamine.
Side effects
- Esketamine: Can cause dissociation, dizziness, nausea, or sedation. That’s why Spravato is only given in certified clinics under a strict FDA Risk Evaluation and Mitigation Strategy (REMS) monitoring program. Long-term ketamine use also raises concerns about tolerance, dependence, and cognitive effects.
- Accelerated TMS: Side effects are usually mild and temporary—scalp discomfort, headache, facial twitching, or fatigue—and don’t involve altered consciousness.
FDA status
- Esketamine (Spravato): FDA-approved for treatment-resistant depression and for adults with MDD and acute suicidal thoughts (when combined with an oral antidepressant).
- IV ketamine: FDA-approved as an anesthetic, but its use for mental health is off-label.
- Accelerated TMS: Select protocols (including SAINT and BrainsWay’s SWIFT Deep TMS) are FDA-cleared for treatment-resistant depression.
Insurance coverage
- IV ketamine: Rarely covered, since it’s off-label for depression.
- Spravato: Covered by many commercial and government plans, but approval often requires meeting strict criteria.
- Accelerated TMS: Coverage is growing but still plan-dependent, usually requiring prior treatment failure and medical justification.
Accelerated TMS vs. electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) works by delivering controlled electrical stimulation to trigger a brief seizure while you’re under general anesthesia. For people who are suicidal, can’t tolerate medications, or haven’t responded to anything else, ECT is still considered the gold standard.
That said, power comes with trade-offs. “More intensive options like ECT may act faster for severe cases,” says Dr. Hanlon, “but [they] involve anesthesia and greater side-effect concerns.”
Treatment timeline
- ECT: Typically given 2–3 times per week for 6–12 sessions
- Accelerated TMS: Multiple short sessions per day over just 5–6 days, possibly with follow-up sessions depending on the protocol.
Effectiveness
For moderate to severe depression, ECT is very effective, with a response rate of 73% and remission rate of 51%. In a minority of people with treatment resistant depression, it can produce a rapid (think: almost immediate) reduction in depressive symptoms and suicidal ideation. However, many people with treatment resistant depression don’t respond until after 6–8 treatments spread over several weeks.
Accelerated TMS shows strong remission and response rates in treatment-resistant depression—up to 79% remission in SAINT studies and 80% response with accelerated Deep TMS.
While one study found ECT reduced depression scores more than standard TMS, it didn’t compare ECT to accelerated TMS, making direct conclusions tricky.
Side effects
- ECT: Common side effects include headache, nausea, muscle aches, and confusion. In rare cases, people experience retrograde amnesia (difficulty recalling past memories). Efforts to speed up ECT by delivering multiple treatments in a single day have led to unacceptable cognitive side effects.
- Accelerated TMS: Side effects are usually mild and temporary, such as scalp discomfort, headaches, facial muscle twitching, or fatigue—without cognitive impairment or anesthesia.
FDA status
- ECT: FDA-approved for catatonia and severe major depressive episodes associated with major depressive disorder or bipolar disorder.
- Accelerated TMS: Select protocols, including SAINT and BrainsWay’s SWIFT Deep TMS, are FDA-cleared for treatment-resistant depression.
Insurance coverage
Most insurance plans at least partially cover ECT. Coverage for accelerated TMS is expanding but remains plan-dependent, typically requiring prior treatment failure and documentation of medical necessity.
Accelerated TMS isn’t a replacement for every depression treatment, but it offers a compelling option for people who want faster relief, fewer side effects, or a non-medication approach. As research evolves and access expands, it’s becoming an increasingly important part of the depression treatment landscape.
Is accelerated TMS safe? What are the side effects?
When it comes to TMS therapy, safety is one of its biggest selling points. “Yes, accelerated TMS is generally very safe,” says Dr. Hanlon. It’s “well tolerated, and most people are able to return to their normal activities right after a session,” she adds.
One major advantage of TMS overall is that it’s targeted and localized. Because it stimulates specific brain circuits rather than affecting the whole body, it avoids many of the systemic side effects commonly associated with medications.
That said, no medical treatment is completely risk-free. The reassuring part? Most side effects are mild, temporary, and similar to standard TMS, according to Dr. Hanlon. Side effects “can include scalp discomfort during treatment, headaches, facial muscle twitching, or feeling tired later in the day,” she says. These symptoms often ease as treatment goes on and are typically easy to manage with simple adjustments.
Serious side effects, such as seizures, are rare and occur at rates similar to standard TMS. Some data estimates a seizure risk of about 7 in 100,000 treatment sessions in traditional TMS. When seizures do occur, they’re usually brief—often under a minute—and don’t lead to lasting complications.
In accelerated TMS, “seizures are extremely uncommon when patients are properly screened,” says Dr. Hanlon. That’s why clinics must carefully evaluate patients with factors that could raise seizure risk, including certain medical conditions, substance use, or age-related considerations.
Clinics that provide TMS are also trained and equipped to manage seizures should they occur—another layer of safety built into care.
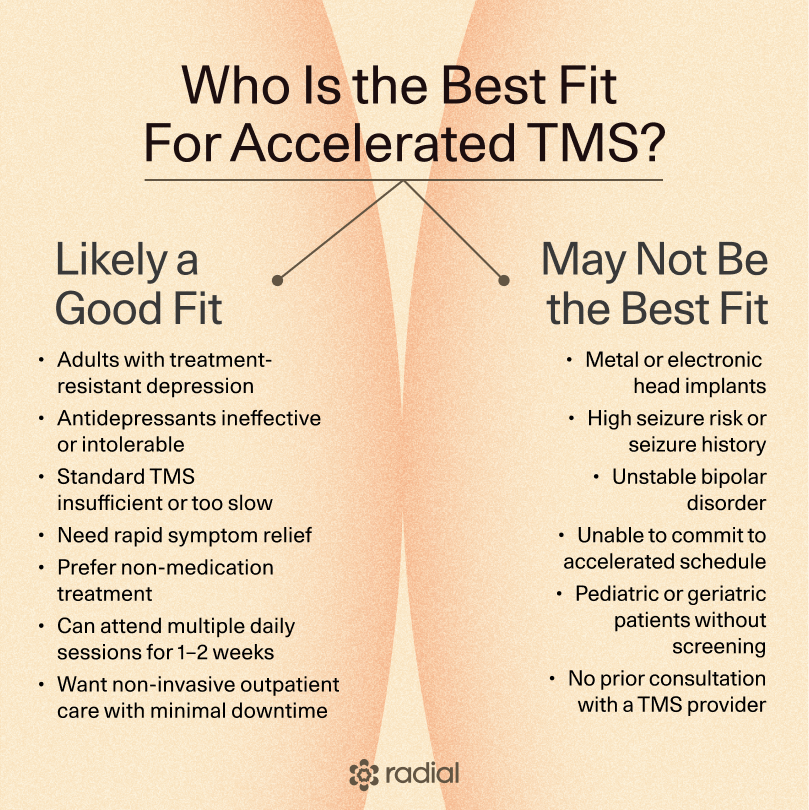
Who is a good candidate for accelerated TMS?
For the right person, accelerated TMS can be truly life-changing. In general, it’s safe and well tolerated, with side effect and seizure rates similar to standard TMS.
“Accelerated TMS can be a great option for adults with depression—especially if medications haven’t helped enough or caused unwanted side effects,” says Dr. Hanlon. In highly treatment-resistant cases, some studies have reported response rates as high as 90.5%, though others show results closer to standard daily TMS.
According to Dr. Hanlon, it’s also appealing for people who:
- Want a non-medication treatment
- Like the idea of finishing therapy faster
- Can commit to multiple sessions per day
Because accelerated TMS works more quickly, it may be especially helpful for people who need rapid symptom relief, including:
- Patients with acute suicidal thoughts
- Those with serious medical conditions who need fast-acting support
- People traveling for treatment or seeking care outside their home community
Who may not be a good candidate?
On the flip side, accelerated TMS isn’t for everyone. “Some people may not be the best fit or may need extra screening first,” says Dr. Hanlon.
This includes individuals with:
- Certain metal or electronic implants in or near the head
- A history of seizures
- Medical conditions that increase seizure risk
- Bipolar disorder (which requires careful evaluation, since brain stimulation can affect mood stability)
“Pregnancy and other medical issues aren’t always deal breakers,” Dr. Hanlon adds, “but they should always be discussed with the treatment team.”
The best way to know if accelerated TMS is right for you is to talk with a trained provider who can review your history, assess risks, and answer your questions, says Dr. Hanlon. A personalized conversation is the safest place to start.
What is an accelerated TMS session like?
You’re not alone if “magnetic pulses to the brain” sounds intimidating—or like something out of a futuristic movie. Still, the reality is much less dramatic. Accelerated TMS is non-invasive and safe for most people. Here, Dr. Hanlon gives us a clear, no-mystery look at what a real SWIFT Deep TMS protocol session is like, so you know exactly what you’re walking into.
Before the session
Because no two brains are the same, every accelerated TMS visit starts with personalization, says Dr. Hanlon.
- You’ll sit in a comfortable chair while a TMS helmet is gently placed on your head.
- A technician delivers light tapping pulses to find your motor threshold (the lowest level of stimulation needed to activate brain cells). This helps fine-tune the dose for your brain.
- You’ll wear hearing protection the whole time (the machine makes a loud clicking sound).
Once that’s done, you’re ready to go.
During treatment
With the SWIFT Deep TMS protocol, treatment happens in multiple quick sessions rather than one long stretch.
- You’ll receive five short sessions per day, each lasting about 10 minutes.
- Sessions are spaced roughly 50 minutes apart, so the full visit takes about 4.5–5 hours—usually manageable as a half-day commitment.
“The acute phase includes six half-day visits, which can be scheduled flexibly over a two-week period,” says Dr. Hanlon. After that comes a lighter follow-up phase: once a week for four weeks, with two sessions per visit (about 90 minutes total).
After each session
No anesthesia means no downtime. Most people feel well enough to drive themselves home, return to work, or go about their day right away.
How much does accelerated TMS cost? Is it covered by insurance?
This is where things get a little complicated (and expensive). Right now, insurance coverage is one of the biggest barriers to accelerated TMS. The good news: most major insurance companies do cover standard TMS and Deep TMS (though usually after someone has tried and not responded to multiple antidepressants), says Dr. Hanlon. The catch? There’s still “very limited insurance coverage for multiple sessions per day,” she says.
That said, momentum is building. Dr. Hanlon notes there’s been some encouraging progress with insurers, and coverage is likely to expand in the future. Some payers are beginning to consider accelerated TMS when traditional schedules haven’t worked, but approval depends heavily on your specific plan and medical necessity.
If insurance doesn’t cover it, brace yourself for a higher price tag. Accelerated TMS is pricey (typically costing between $17,000 and $23,000 for a course of treatment), reflecting the intensive schedule and staffing required. Costs can climb further if advanced tools are used. For example, the SAINT protocol relies on functional MRI to personalize targeting—an approach that may improve precision but also adds expense, notes Dr. Hanlon.
While the sticker shock is real, there may be options. Some clinics offer financial support to reduce the burden. Radial, for instance, provides financial hardship programs, accepts HSA/FSA cards, offers buy-now-pay-later options through partners like CareCredit and Wisetack, and can set up flexible payment plans when needed.
The gist: Accelerated TMS isn’t cheap, and insurance coverage is still catching up, but access is improving. If you’re interested, it’s worth asking both your provider and insurer about coverage options, alternatives, and payment plans that could make treatment more feasible.
Where is accelerated TMS available?
Accelerated TMS is the new kid on the block. Standard TMS has been around for years, but accelerated versions are still rolling out, so you won’t find them at every clinic just yet.
A simple Google search for “accelerated TMS near me” can turn up clinics or hospital programs that offer it. If you’re specifically interested in SAINT TMS, Magnus Medical runs a locator tool (Radial clinics show up there, too). Another route? Clinical trials. Some people access accelerated TMS through open research studies.
Found a few options? Now it’s time to vet them. Not all accelerated TMS is the same, so asking the right questions matters. When you talk to a provider, consider asking:
- Which protocol do you offer? Accelerated TMS comes in different flavors. Make sure they can explain which approach they use and why it might (or might not) be a good fit for you.
- Can you help with insurance? Ask if there’s a care coordinator or staff member who helps navigate coverage and prior authorizations.
- What if I’m paying out of pocket? See whether they offer payment plans, financing options, or financial assistance.
- Do you offer add-on support? Some clinics pair TMS with therapy or other treatments to boost results—worth asking about.
Doing a little homework upfront can help you find the right clinic.
The bottom line
Accelerated TMS isn’t a magic fix, but it is a promising option for people who need relief sooner and haven’t found it with meds alone. By delivering a powerful, evidence-based treatment in a much shorter timeframe, it offers a new path forward for people stuck waiting weeks (or months) to feel better.
If you’re struggling with depression and wondering whether accelerated TMS could make sense for you, you don’t have to figure it out alone. Radial helps connect you with licensed clinicians—virtually or in person—who specialize in fast-acting, science-backed treatments and will work with you to build a personalized plan. When you’re ready to explore your options, Radial is here to help you take the next step.
Key takeaways
- Accelerated TMS compresses weeks of treatment into days, delivering multiple short sessions per day with the goal of faster symptom relief.
- Early research shows high response and remission rates, even in people with treatment-resistant depression—though more large-scale studies are still needed.
- Side effects are generally mild and temporary, especially compared to medications, ketamine, or ECT—and there’s no anesthesia or downtime.
- Not all accelerated protocols are the same, so outcomes depend on factors like session timing, total dose, and the specific approach used.
- Insurance coverage is growing but inconsistent, making provider support and financial navigation an important part of the process.
Frequently asked questions (FAQs)
Is accelerated TMS covered by insurance?
Sadly, coverage is still limited. Most major insurers cover standard TMS and Deep TMS, but many don’t yet routinely cover multiple sessions per day, says Dr. Hanlon. Some plans may approve it on a case-by-case basis if standard treatments haven’t worked and medical necessity is documented. Coverage varies a lot by plan, so it’s worth asking a provider who can help you navigate prior authorization or alternatives.
Is accelerated TMS safe?
Yes—accelerated TMS is generally very safe and well tolerated, with side effects similar to standard TMS. The most common ones are mild and temporary—things like scalp discomfort, headaches, facial muscle twitching, or feeling tired later in the day. Serious side effects, such as seizures, are rare, especially when patients are properly screened.
Is accelerated TMS FDA approved?
Yes—specific accelerated protocols are FDA-cleared. This includes approaches like SAINT TMS and BrainsWay’s SWIFT Deep TMS protocol for treatment-resistant depression. That said, not every accelerated schedule is FDA-cleared yet, and research is still evolving to determine the best dosing and delivery methods.
Deep dive recommendations:
- The Frontier Psychiatrist Podcast. Episode How Did Rapid Remission from Depression Become the New Standard of Care? S2. E1 https://podcasts.apple.com/us/podcast/how-did-rapid-remission-from-depression-become-the/id1577248149?i=1000694328719
- The Frontier Psychiatrist Podcast. Accelerated Transcranial Magentic Stimulation (aTMS) explained. https://podcasts.apple.com/us/podcast/accelerated-transcranial-magnetic-stimulation-atms/id1577248149?i=1000655423684
- The Carlat Report Podcast. How to Find SAINT TMS. https://podcasts.apple.com/us/podcast/how-to-find-saint-tms/id1463414537?i=1000739085878
- The Carlat Report Podcast. A More Powerful Antidepressant. https://podcasts.apple.com/us/podcast/a-more-powerful-antidepressant/id1463414537?i=1000738081222
- The Carlat Report Podcast. How to Explain TMS. https://podcasts.apple.com/us/podcast/how-to-explain-tms/id1463414537?i=1000734998143
Editorial Standards
At Radial, we believe better health starts with trusted information. Our mission is to empower readers with accurate, accessible, and compassionate content rooted in evidence-based research and reviewed by qualified medical professionals. We’re committed to ensuring the quality and trustworthiness of our content and editorial process–and providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. Learn more about our editorial process.
Let's connect
Get started with finding the right treatment for you or someone you care about
Get started



